Dengue Fever Associated Liver Failure
Joanne Mui Ching Tan, Natalie Woon Hui Tan, Koh Cheng Thoon, Chia Yin Chong and Christina Ong
DOI10.21767/2573-0282.100031
Joanne Mui Ching Tan1, Natalie Woon Hui Tan2,3,4,5*, Koh Cheng Thoon2,3,4, Chia Yin Chong2,3,4 Christina Ong3,4,5,6
1Department of Pediatrics, KK Women’s and Children’s Hospital, Singapore
2Infectious Disease Service, Department of Pediatrics, KK Women’s and Children’s Hospital, Singapore
3Yong Loo Lin School of Medicine, National University of Singapore, Singapore
4Duke-NUS Medical School, Singapore
5Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore
6Gastroenterology Service, Department of Pediatrics, KK Women’s and Children’s Hospital, Singapore
- *Corresponding Author:
- Natalie Woon Hui Tan
Infectious Disease Service, Department of Pediatrics, KK Women’s and Children’s Hospital, Singapore
Tel: +65-81217682
E-mail: Natalie.tan.w.h@singhealth.com.sg
Received Date: October 24, 2016; Accepted Date: November 21, 2016; Published Date: November 25, 2016
Citation: Tan JMC, Tan NWH, Ong C, Thoon KC, Chong CY(2016) Dengue Fever Associated Liver Failure. Pediatric Infect Dis 1:31. doi: 10.21767/2573-0282.100031
Abstract
Background: Dengue fever is common in Southeast Asia although liver failure is a rare complication with up to 50% mortality rate reported in children. Objective: To evaluate the characteristics and treatment outcome of dengue fever associated liver failure (DFALF) in a case series of 4 paediatric patients. DFALF was defined as INR>2, regardless of the presence or absence of encephalopathy or INR>1.5 not corrected by Vitamin K in the presence of clinical hepatic encephalopathy, during the course of concurrent dengue infection. Material and methods: Patients with DFALF, admitted to a tertiary paediatric centre in Singapore over a 6 year period (January 2009-December 2015) were identified from the Gastroenterology and Infectious Disease databases. Case records were retrospectively reviewed. Results: Four patients, all boys, age 5 months to 6 years, presented at the acute febrile phase of illness with Dengue Shock Syndrome (severe dengue). Aspartate Transaminase (AST) and Alanine Transaminase (ALT) peaked at day 4-7: median (± 2SD) peak ALT 1871.5 ± 917 u/L, whereas median peak AST 7802.5 ± 5453.8 u/L. Median peak International Normalised Ratio ( INR ), ammonia, lactate were 2.9 ± 1.6, 106 ± 144.6 umol/L, and 7.4 ± 8.4 mmol/L respectively. All patients had hepatomegaly and mild conjugated hyperbilirubinaemia, with median peak total bilirubin 73.5 ± 36.9 umol/L. Two patients received N-Acetylcysteine. One patient received intravenous dexamethasone for dengue associated hemophagocytic lymphohistiocytosis. All recovered fully with supportive treatment based on a well-designed acute liver failure protocol, which comprised of intensive care monitoring, correction of coagulopathy and hypoglycaemia, empirical broad spectrum antibiotic coverage and anti-fungal prophylaxis, gastrointestinal haemorrhage prophylaxis with a histamine-2 receptor antagonist, proton pump inhibitor or sucralfate, and lactulose to reduce hyperammonaemia. Liver function significantly improved (ALT<500 u/L) at a median of 6.5 ± 2 days from onset of liver failure. INR normalized (INR<1.1) at a median of 13.5 ± 6 days of illness. Conclusion: Patients with DFALF can achieve normalisation of liver function and full recovery with early supportive treatment.
Keywords
Children; Dengue fever; Liver failure
Introduction
Dengue fever is a pandemic viral disease carried by mosquitoborne flavivirus. The World Health Organisation (WHO) estimated that 50 million dengue infections occur annually. In the last 50 years, the incidence has increased 30 fold with geographical distribution to about 100 countries, making it the most rapidly spreading arboviral infection [1]. Liver failure is a rare, recognised complication of dengue fever. Dengue fever associated liver failure (DFALF) was defined as International Normalized Ratio (INR)>2 during the course of illness, regardless of the presence or absence of encephalopathy or INR>1.5 not corrected by Vitamin K in the presence of clinical hepatic encephalopathy [2], with concurrent dengue infection. In Cuba and Singapore, sequential dengue infections at long intervals produced unusually severe disease in adults [3]. The 2005 dengue epidemic in Singapore reported a total of 14,006 cases of dengue infection in which 13625 cases were dengue fever and 381 cases of dengue haemorrhagic fever, including 27 deaths. This gave rise to an incidence rate of 322.6 in 100,000 and a case fatality rate of 0.19% [4]. Despite efforts of disease control, dengue fever continues to be a significant public health concern. Dengue fever can present as self-limiting acute febrile illness or the more severe forms with dengue shock syndrome, bleeding and other major organ involvement. Hepatitis is common and can be found in 60-90% of dengue infected patients [5-7]. Elevation of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) is prominent in acute dengue illness. The World Health Organization (WHO) 2009 dengue guidelines defined AST or ALT ≥ 1000 units/liter (U/L) as a criterion for severe dengue. Deranged liver enzymes are usually in the mild to moderate range and severe hepatitis with transaminases 10 times above the upper limit of normal is less common at 3-11% [6,7]. The aim of our study was to describe the characteristics and clinical outcome of DFALF in children.
Material and Methods
Patients with DFALF, admitted to KK Women and Children’s Hospital, the main tertiary paediatric centre in Singapore over a 6 year period (January 2009-December 2015) were identified from the Gastroenterology and Infectious Disease databases. The case notes were retrospectively reviewed for demographic data, clinical presentation, investigations, management and outcome. Data analysis was conducted using Microsoft Excel 2010. This study was approved by the Institutional Review Board, Sing health Healthcare Group, Singapore. All authors declared that there is no support from any organisation for the submitted work; no financial relationships with any financial organisations that might have interest in the submitted work; no other relationships of activities that could appear that could have influenced the submitted work.
Results
Four male patients aged 5 months to 6 years, presented at the acute febrile phase of illness with Dengue Shock Syndrome (severe dengue) and subsequently developed DFALF. Two patients were Indonesians who acquired dengue infection in Batam, Indonesia. One was a Filipino, who lived locally but acquired dengue infection while he was back in the Philipines for holiday. One Chinese patient acquired dengue infection locally. Out of these 4 patients, three patients had primary dengue whereas one patient had secondary dengue.
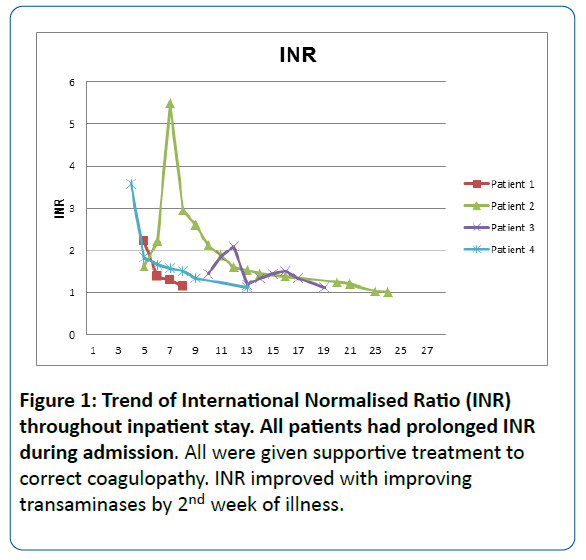
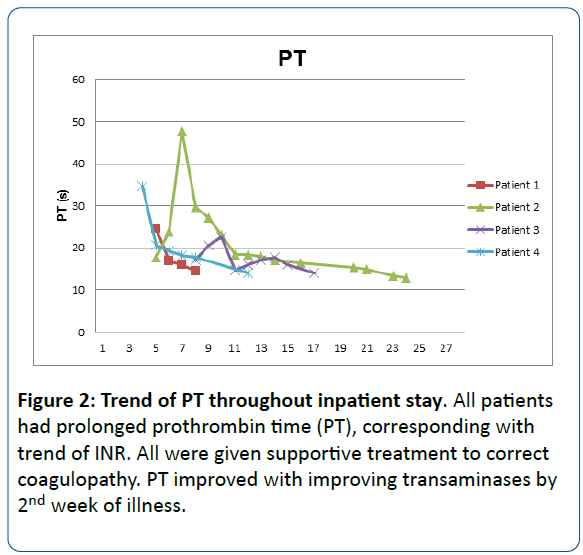
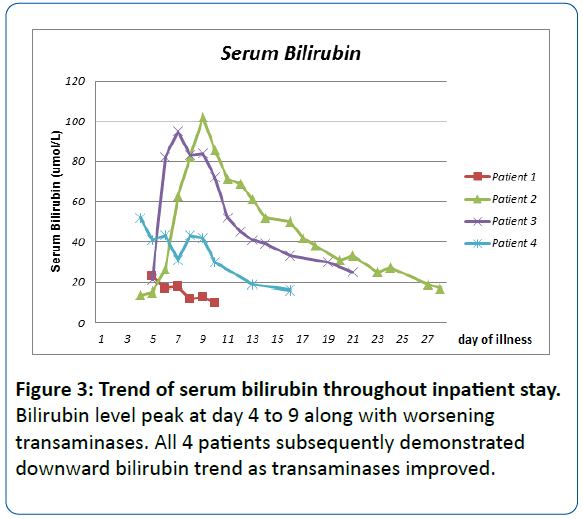
Three out of four patients had hepatic encephalopathy. Acute liver failure occurred at a median of 5.5 ± 3 days after the onset of fever with peak of AST and ALT at day 4 to 7. For our case series, median peak ALT for all 4 patients was 1871.5 ± 917 u/L, whereas median peak AST was 7802.5 ± 5453.8 u/L. Median peak International Normalised Ratio (INR) 2.9 ± 1.6, ammonia 106 ± 144.6 umol/L and lactate 7.4 ± 8.4 mmol/L. All patients developed hepatomegaly with deranged transaminases and eventually resolved with normalisation of transaminases. All had mild conjugated hyperbilirubinaemia: median total bilirubin 73.5 ± 36.9 umol/L, median peak direct bilirubin 50.5 ± 25.5umol/L. Table 1 shows the demographic, clinical and laboratory characteristics of all 4 cases on admission. Table 2 shows the clinical progression, management and outcome of all 4 patients.
The mainstay of treatment included correction of coagulopathy and hypoglycaemia, empirical broad spectrum antibiotic coverage and fungal prophylaxis, gastrointestinal haemorrhage prophylaxis with a histamine-2 receptor antagonist, proton pump inhibitor or sucralfate,and lactulose to reduce hyperammonaemia. Two out of four patients, with AST>10,000 U/L received intravenous N-acetylcysteine for 1 week as part of the medical therapy for acute liver failure without adverse effects.
One patient received intravenous dexamethasone for dengue associated hemo-phagocytic lympho-histiocytosis (HLH), a rare but increasingly reported complication. He presented with fever, hepato-splenomegaly and coagulopathy with hypofibrinogenaemia, hyper-triglcaeridaemia, hyper-ferritinaemia and bone marrow aspirate showed haemo-phagocytosis.
One patient had dengue-associated meningoencephalitis as evident by clinical presentation of seizures and encephalopathy with presence of leptomeningeal enhancement on Magnetic Resonance Imaging of the brain. He also developed acute leukaemoid reaction (maximum total white of 26.62 X 10(9)/L) with 3% blast cells on initial blood film which subsequently resolved. All 4 patients received supportive medical treatment with recovery of liver function and were discharged well.
Liver function gradually improved with support and our patients achieved ALT<500 u/L at median of 6.5 ± 2 days from onset of liver failure. INR normalised (INR<1.1) at median 13.5 ± 6 days of illness. Figures 1 and 2 show the trend of Alanine aminotransferase (ALT) and Aspartate aminotransferase (AST) respectively over the length of inpatient stay. Supplementary figures 1-3 reflect the trend of INR, Prothrombin time (PT) and serum bilirubin throughout inpatient stay.
Discussion
Dengue fever continues to be a major challenge to public health in South-East Asia. Fatality rates of dengue fever in South East Asia are 1%, with higher reported rates of 3-5% in local outbreaks in India, Indonesia and Myanmar. Of these, at least 90% are children younger than 15 years [1]. Studies from India and Thailand suggested that dengue infection was the most important cause of acute hepatic failure in children contributing to 18.5% and 34.3% of the cases respectively [8,9]. Studies in Taiwan and Vietnam reported DFALF to occur in 3 of 270 patients in Taiwan [7] and 5 of 644 patients in Vietnam [10]. In Malaysia, 8 out of 20 paediatric patients with Dengue Haemorrhagic Fever developed liver failure, 1 died, and the rest achieved full recovery [11].
In our series of 4 patients, we found that acute liver failure occurred at a median of 5.5 days after the onset of fever. These findings are comparable to other case reports which reported acute liver failure at 5 to 14 days from the onset of fever [12-14]. The AST had been reported to peak on day 7 to 8 of illness and the ALT lags behind AST in time and magnitude [7]. Mechanisms of dengue associated liver injury is postulated to be contributed by direct viral injury or dysregulated host immune response to liver cells, hypoxic ischaemic injury caused by circulatory compromise or localised vascular leakage inside the liver. Histological findings of hepatocyte necrosis at zone two and councilman bodies have been reported [15].
In dengue fever associated liver failure, AST levels are more often elevated than ALT levels, a pattern that may be useful to distinguish from the diagnosis of other classical hepatotropic viruses such as Hepatitis A, B or C infection, where ALT levels were usually higher than AST level. This was postulated to be due to AST released from damaged myocytes [7]. All 4 patients in our case series had markedly elevated serum transaminases at values above 10 times the upper limit of normal, with AST levels more elevated than ALT by 1.4 to 5.5 times. These abnormal liver enzymes improved rapidly with supportive management. A study involving 8 adult patients with DFALF by Tan et al in 2013 reported that ALT decreased to <500 u/L after median of 5.5 days [16]. In comparison, our 4 patients achieved the same level at median of 6.5 days.
Besides supportive management of patients with dengue related liver failure, N-acetylcysteine (NAC) therapy, though not routinely indicated in non-acetaminophen related acute liver injury, have been found to be beneficial in some studies. A retrospective analysis by Senanayake et al. on 7 paediatric patients with DFALF showed survival advantage if patients with early (grade I or II) liver failure were treated with NAC therapy at 100 mg/kg [17]. Two of our patients, haemodynamically unstable, with AST>10,000 u/L, were treated with continuous intravenous NAC infusion therapy at 100 mg/kg/day for 1 week. Both demonstrated rapid decline in liver transaminases and improvement in coagulation profile, followed by clinical improvement. There were no adverse effects noted.
HLH should be considered in patients with dengue fever with prolonged fever, worsening cytopenias and multiorgan complications. The pathogenesis of both dengue infection and HLH is related to increased secretion of pro-inflammatory cytokines, thus forming the pathogenic link between the two [18]. The general principles of management of patients with secondary HLH includes treatment of the triggering cause, supportive management, corticosteroid and, if required, chemotherapy [19].
A case series comprising of 8 patients fulfilling the criteria of dengue associated HLH, achieved full recovery with a novel short course of Dexamethasone. The patients were started on parenteral dexamethasone of 10 mg/m2/day in 3 to 4 divided doses and continued for 7 days and completed a total of 4 weeks with tapering doses [20]. We saw a good outcome in our 1 patient with dengue related HLH, who responded well to steroid therapy only. No chemotherapy was required. Further studies should be done to explore this as standard therapy for dengue associated HLH.
A retrospective study in Thailand reported up to 50% mortality in the paediatric population with DFALF, much higher than the overall fatality rate of 0.3% from dengue infection [21]. Similar to our experience, Tan et al reported 100% survival from standard medical therapy in 8 adult patients with DFALF in Malaysia [16], which included nursing with head of bed elevated at 30° , initiation of enteral nutrition whenever possible, fluid management with crystalloids and colloids, correction of thrombocytopenia and coagulopathy and broad spectrum antibiotics. All 4 patients in this case series fulfilled at least 1 to 2 out 3 poor prognostic factors of King’s College Hospital criteria for poor prognosis.
Causes of acute liver failure such as drug reaction and hepatitis B, less than 11 years of age and higher grades of encephalopathy had poorer survival rates [22]. Despite factors associated with poor prognosis, with intensive care monitoring and supportive treatment, all 4 patients showed improvement in liver function within 1 week. This suggests that DFALF is selflimiting, supportive treatment allows time for liver to recover naturally. N-acetylcysteine is a safe and effective drug in ameliorating acute liver failure from dengue fever, especially in patients with fulminant liver failure who are haemodynamically unstable or does not fulfil criteria for liver transplantation. With early supportive treatment, patients with DFALF can achieve normalisation of liver function and full recovery.
References
- World Health Organisation (2009) Dengue-guidelines for diagnosis, treatment, prevention and control. Switzerland: WHO Press.
- Squires RH Jr, Shneider BL, Bucuvalas J (2006) Acute liver failure in children: the first 348 patients in the pediatric acute liver failure study group. J Pediatr. 148: 652-658
- Halstead SB (2007) Dengue. Lancet 370: 1644-52.
- Koh BK, Ng LC, Kita Y (2008) The 2005 dengue epidemic in Singapore: epidemiology, prevention and control. Ann Acad Med Singapore 37: 538-45
- Nguyen TL, Nguyen TH, Tieu NT (1997) The impact of dengue haemorrhagic fever on liver function. Res Virol 1948: 273-277.
- De Souza LJ, Nogueira RM, Soares LC (2007) The impact of dengue on liver function as evaluated by aminotransferase levels. Braz J Infect Dis 11: 407-10.
- Kuo CH, Tai DI, Chang Chien CS, Lan CK, Chiou SS, et al. (1992) Liver biochemical tests and dengue fever. Am J Trop Med Hyg 47: 265-270.
- Petdachai W (2005) Hepatic dysfunction in children with dengue shock syndrome. Dengue Bull 29: 112-117.
- Wahid SF, Sanusi S, Zawawi MM (2000) A comparison of the pattern of liver involvement in dengue haemorrhagic fever with classic dengue fever. Southeast Asian J Trop Med Public Health 31: 259-263.
- Trung DT, Thao le TT, Hung NT, Vinh NN (2010) Liver involvement associated with dengue infection in adults in Vietnam. Am J Trop Med Hyg 83: 774-780.
- Lum LC, Lam SK, George R (1993) Fulminant hepatitis in dengue infection. Southeast Asian J Trop Med public health 24: 467-471
- Viswanathan S, Iqbal N, Anemon PP (2010) Fatal fulminant hepatic failure in a diabetic with primary dengue. J Trop Med 2010: 413561
- Subramanian V, Shenoy S, Joseph AJ (2005) Dengue haemorrhagic fever and fulminant hepatic failure. Dig Dis Sci 50: 1146-1147
- Souza LJ, Coelho JM, Silva EJ (2008) Acute hepatitis due to dengue virus in a chronic hepatitis patient. Braz J Infect Dis 12: 45-49
- Seneviratne SL, Malavige GN, de Silva HJ (2006) Pathogenesis of liver involvement during dengue viral infections. Trans R Soc Trop Med Hyg 100: 208-214.
- Seok-Siam Tan, Muhamad Adam Bujang (2013) The clinical features and outcomes of acute liver failure associated with dengue infection in adults: a case series. Braz J infect Dis 17: 164-169
- Senanayake MP, Jayamanne MD, Kankananarachchi I (2013) N-acetylcysteine in children with acute liver failure complicating dengue viral infection. Ceylon Med J 58: 80-82.
- UmbreenArshad, SaqibQayyum Ahmad, Fauzia Khan (2015) Haemophagocytic lymphohistiocytosis in a patient with dengue fever. HemaotoOncol Stem Cell Ter 8: 4
- Jordan MB, Allen CE, Weitzman S (2011) How I treat hemophagocytic lymphohistiocytosis. Blood 118: 4041-52.
- Priyankar Pal, PrabhasPrasunGiri, AV Ramanan (2014) Dengue Associated Hemophagocytic Lymphohistiocytosis; A Case Series. Indian Pediatr 51: 496-497.
- Chongsrisawat V, Hutagalung Y, Poovorawan Y (2009) Liver function test results and outcomes in children with acute liver failure due to dengue infection. Southeast Asian J Trop Med Public Health 40: 47-53.
- O’Grady J, Alexander G, Hayllar K, (1989) Early indicators of prognosis in fulminant liver failure. Gastroenterology 97: 439-445.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences