Abstract
Dengue Fever Associated Liver Failure
Background: Dengue fever is common in Southeast Asia although liver failure is a rare complication with up to 50% mortality rate reported in children. Objective: To evaluate the characteristics and treatment outcome of dengue fever associated liver failure (DFALF) in a case series of 4 paediatric patients. DFALF was defined as INR>2, regardless of the presence or absence of encephalopathy or INR>1.5 not corrected by Vitamin K in the presence of clinical hepatic encephalopathy, during the course of concurrent dengue infection. Material and methods: Patients with DFALF, admitted to a tertiary paediatric centre in Singapore over a 6 year period (January 2009-December 2015) were identified from the Gastroenterology and Infectious Disease databases. Case records were retrospectively reviewed. Results: Four patients, all boys, age 5 months to 6 years, presented at the acute febrile phase of illness with Dengue Shock Syndrome (severe dengue). Aspartate Transaminase (AST) and Alanine Transaminase (ALT) peaked at day 4-7: median (± 2SD) peak ALT 1871.5 ± 917 u/L, whereas median peak AST 7802.5 ± 5453.8 u/L. Median peak International Normalised Ratio ( INR ), ammonia, lactate were 2.9 ± 1.6, 106 ± 144.6 umol/L, and 7.4 ± 8.4 mmol/L respectively. All patients had hepatomegaly and mild conjugated hyperbilirubinaemia, with median peak total bilirubin 73.5 ± 36.9 umol/L. Two patients received N-Acetylcysteine. One patient received intravenous dexamethasone for dengue associated hemophagocytic lymphohistiocytosis. All recovered fully with supportive treatment based on a well-designed acute liver failure protocol, which comprised of intensive care monitoring, correction of coagulopathy and hypoglycaemia, empirical broad spectrum antibiotic coverage and anti-fungal prophylaxis, gastrointestinal haemorrhage prophylaxis with a histamine-2 receptor antagonist, proton pump inhibitor or sucralfate, and lactulose to reduce hyperammonaemia. Liver function significantly improved (ALT<500 u/L) at a median of 6.5 ± 2 days from onset of liver failure. INR normalized (INR<1.1) at a median of 13.5 ± 6 days of illness. Conclusion: Patients with DFALF can achieve normalisation of liver function and full recovery with early supportive treatment.
Author(s):
Joanne Mui Ching Tan, Natalie Woon Hui Tan, Koh Cheng Thoon, Chia Yin Chong and Christina Ong
Abstract | Full-Text | PDF
Share this

Google scholar citation report
Citations : 230
Pediatric Infectious Diseases: Open Access received 230 citations as per google scholar report
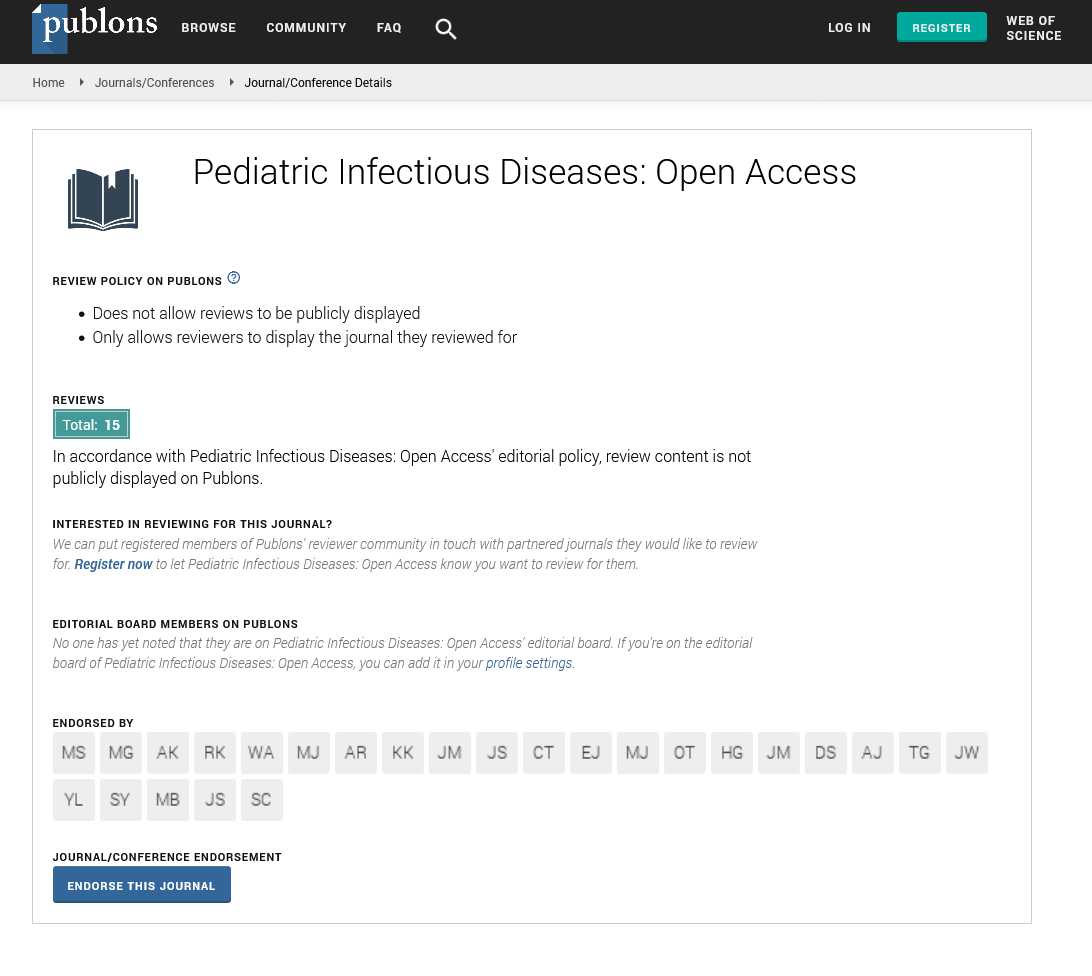
Pediatric Infectious Diseases: Open Access peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- Cosmos IF
- Secret Search Engine Labs
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences