Role of Ommaya Reservoir in Paediatric Hydrocephalus: Experience in Bangladesh Medical College Hospital from 2019-2021
Hamid R*, Gomes VC, Huda N, Khan AR, Chowdhury M and Azam I
Published Date: 2022-08-18Hamid R1*, Gomes VC1, Huda N1, Khan AR1, Chowdhury M1and Azam I2
1Department of Science, Bangladesh Medical College Hospital, Dhaka, Dhanmondi, Bangladesh
2Department of Medical Science, Dhaka Medical College Hospital, Dhaka, Bangladesh
- *Corresponding Author:
- Hamid R Department of Science, Bangladesh Medical College Hospital, Dhaka, Dhanmondi, Bangladesh, Tel:8801715027000; E-mail:rezina.hamid@gmail.com
Received date: June 11, 2022, Manuscript No. IPPIDO-22-13778; Editor assigned date: June 13, 2022, PreQC No. IPPIDO-22-13778 (PQ); Reviewed date: June 27, 2022, QC No. IPPIDO-22-13778; Revised date: August 11, 2022, Manuscript No. IPPIDO-22-13778 (R); Published date: August 18, 2022, DOI: 10.36648/2573-0282.7.9.32
Citation: Hamid R, Gomes VC, Huda N, khan AR, Chowdhury M, et al. (2022) Role of Ommaya Reservoir in Paediatric Hydrocephalus: Experience in Bangladesh Medical College Hospital from 2019-2021. Pediatr Infect Dis Vol:7 No:9
Abstract
Objective: Aim of the study is to evaluate the efficacy of ommaya reservoir in all types of pediatric hydrocephalus and at the same time its safety for repeated aspirations or long term retention of reservoir in the body.
Method: Between 2019-2021, n=33 consecutive cases of reservoir implantation were taken into study irrespective of etiology of hydrocephalus. These were mostly placed along with endoscopic third ventriculostomy and some were placed as an intermediary procedure to combat shunt complications in emaciated infants. Cerebrospinal fluid aspiration was done in case of failed endoscopic third ventriculostomy and frequency of aspiration was depended upon the production of cerebrospinal fluid. Acetazolamide was routinely administered in each patient to reduce the frequency of aspiration. Most of the patient required ventriculoperitoneal shunt while they had sufficient body weight and few required no surgery.
Results: Average age at presentation was 76.88 days. All the neonates and infants had less weight in terms of their age. 42.4% babies needed aspiration 2 times per week. Among all cases, 9.1% developed reservoir complications. Complications were not related to number and volume of aspiration or duration of reservoir in body. 2 patients had died after one year of reservoir implantation due to unrelated diseases. Out of the 31 survivors, 3 patients did not need any further aspiration and 19 patients needed ventriculoperitoneal shunt, but reservoir was kept in situ for future emergency. Rest of them is waiting for definitive shunt procedure. Other findings include low socioeconomic group was more prone to low birth weight and they carried the burden of congenital hydrocephalus and meningomyelocele. Most affected babies had their prenatal period in arsenic affected areas in Bangladesh. Overall folic acid supplementation was started after the formation of neural tube irrespective of socioeconomic status.
Conclusion: Ommaya reservoir placement along with endoscopic third ventriculostomy plays a vital role in delaying shunt in endoscopic third ventriculostomy failure. It is a ‘time buying’ procedure until baby has sufficient weight for successful shunt surgery. It has been found very effective intermediary intervention for managing shunt infection and it also helps revival of a channel in shunt obstruction.
Keywords
Ommaya reservoir; Repeated and prolonged CSF aspiration
Abbreviation
CSF: Cerebro Spinal Fluid; ETV: Endoscopic Third Ventriculostomy; V-P Shunt: Ventriculo Peritoneal Shunt; EVD: External Ventricular Drain; OFC: Occipito Frontal Circumference; ACTH: Adrenocorticotropic Hormone; ICP: Intracranial Pressure; PHH: Post Hemorrhagic Hydrocephalus; CNS: Central Nervous System; IVT: Intra Ventricular Therapy
Introduction
Hydrocephalus is the distension of the brain ventricle due to inadequate passage of CSF from its site of production within the cerebral ventricles to its site of absorption into the systemic circulation or disturbance of CSF absorption and rarely excess secretion [1,2]. CSF is constantly made by CNS, which carries nutrients, washes away debris and acts as a cushion for CNS. After its production from choroid plexus (80%) and ependymal lining, CSF flows through ventricular pathway and absorbed into sub arachnoid space prior to getting absorbed in blood through arachnoid granulations [3]. Hydrocephalus results as a congenital blockage to the pathway or due to post inflammatory adhesion of sub arachnoid space or destruction of arachnoid granulations. There are other varieties of acquired hydrocephalus. The incidence of hydrocephalus in the new born varies from 0.2-0.5 per 1000 birth and almost half of this children born prematurely [4,5]. The commonest cause of hydrocephalus is obstructive hydrocephalus due to aqueduct stenosis and for communicating or non-obstructive hydrocephalus includes post infective and post hemorrhagic hydrocephalus with an incidence of 0.9 to 1.5 per 1000 births [6,7]. Most often used definitive permanent treatment option for hydrocephalus is shunt that enables drainage of CSF in the other body cavity commonest being the ventriculo peritoneal shunt. But unfortunately a great number of children failed to tolerate shunt system in the body due to poor physical condition. As majority of the babies are pre mature and underweight, they are highly prone to skin dehiscence and skin infection [8]. Shunt infection rate varies from 10% to 22% and approximately 90% of the infections usually occur one month after surgery [9]. Different studies have already revealed in their studies that premature birth was independently associated with VP shunt infection due to poorly developed immune system, immaturity of the skin and the probable high density bacteria on the skin of premature infants [10-15]. Also inability to CSF absorption distally in the peritoneum may contribute to shunt failure in this population, so temporary drainage of CSF is often necessary. Other methods of treatment that have been performing in many medical centers all over the world include lumber puncture or trans fontanelle ventricular puncture.
The subcutaneous ommaya reservoir was initially used in 1960 for intraventricular application of medication in adults. However, since 1980 it has been used for evacuation of the cerebrospinal fluid in prematurely born children with PHH [16,17]. This procedure is relatively simple and allows controlled CSF aspiration transcutaneously by monitoring clinical condition of the baby until baby gets fit enough for definitive 10-14 shunt procedure. This reservoir has advantages over repeated lumber punctures and repeated transcortical ventricular puncture. The major complications with reservoir include subcutaneous CSF leakage, cutaneous inflammation, skin necrosis and ventriculitis [18]. Endoscopic third ventriculostomy along with Ommaya reservoir is a well known alternative to VP shunt in treatment of obstructive hydrocephalus in aqueductal stenosis [19]. It also plays crucial role in delaying shunt in malnourished babies.
In our study, we retrospectively evaluated outcome of 34 hydrocephalus babies of various etiology with ommaya reservoir. Most of them were placed along with ETV and rest as an intermediate procedure in managing shunt infection. We studied the durability, early and late complications of ommaya reservoir insertion. We also assessed the consequence of high volume and long-time aspiration of CSF.
From 2016, we were working on the factors responsible for shunt infection in developing countries. In our setting we found shunt infection most commonly occurs in the first year of life and it is the most common complication occurring within 30 days of implantation [20]. The intelligence based medicine also clearly concluded pre maturity, number of shunt revisions and low birth weight have strong role on shunt infection [21].
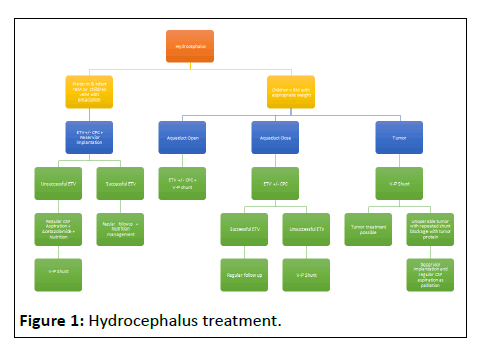
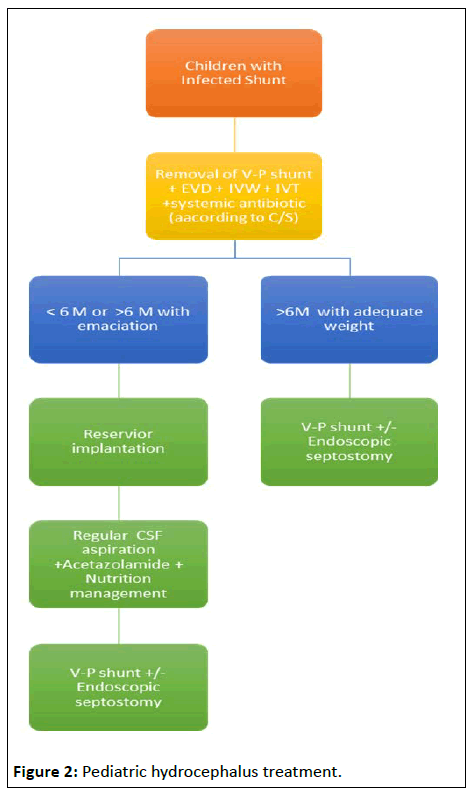
Bangladesh is a developing country and we are progressing slowly but steadily in health sector. Babies often have low birth weight and have got less subcutaneous body fat. This flowchart was developed to delay shunt in any low body weight or emaciated babies. Ommaya reservoir had its unique way to resolve this problem (Figures 1 and 2).
This is the flow chart we follow to treat pediatric hydrocephalus.
After going through the flow chart, one can comprehend the role of Ommaya reservoir in delaying shunt. In this article, we are weighing the cost and benefit of reservoir implantation. The major complications of reservoir implantation are subcutaneous CSF leak, skin sloughing, obstruction and meningitis [22]. The first two occur as a consequence of delaying aspiration, omitting acetazolamide, keeping the baby flat after surgery. Incision over the reservoir and failing to create sufficient subcutaneous pocket fall into territory of poor surgical technique. Meningitis is due to lack of asepsis and prevalent in pre tem, low birth weight category. In this study we evaluated Ommaya reservoir related complication as we are using it in diverse procedure like with ETV and shunt infection.
Aims of the study
• To ascertain the role of ETV+reservoir implantation as a time buying procedure in premature, low body weight and complicated cases.
• To find out the reservoir related complications.
• To see the result of long time aspiration or high volume aspiration of CSF and its relationship with complications.
Objectives of the study
• To see the predominant type of hydrocephalus affecting the patient group.
• To see the gestational period of starting folic acid supplementation irrespective of type of hydrocephalus.
• To observe the geographical role of congenital and spine bifida group.
• To determine the socio economic background of the patients.
Materials and Methods
It is a retrospective, cross sectional study regarding indication, placement, utility and complication of Ommaya reservoir in pediatric hydrocephalus irrespective of its etiology. In this study we took 33 successive cases of reservoir implantation. Ommaya reservoir was placed routinely with ETV, as it acts as a channel for CSF aspiration in case of ETV failure. Most of the patients fell into these criteria. Babies usually present with low body weight, their sub cutaneous fat is poorly developed. In event of ETV failure, we don’t go for immediate VP Shunt. We aspirate CSF at least twice or thrice weekly (depending on formation) in outdoor basis and we routinely prescribe acetazolamide to decrease the production of CSF.
Ommaya reservoir is routinely used to delay shunt insertion in emaciated infants with shunt infection. They are treated by removal of infected tube followed by EVD. They get both parenteral antibiotic and sometimes in intra ventricular route via EVD. When CSF is culture negative we put Ommaya reservoir and discharge them with advice of regular CSF aspiration. We don’t advocate shunt surgery until and unless baby gains sufficient weight. Babies treated with this method showed no infection.
Sometimes we go for re do reservoir placement due to reservoir infection. This always have an intermediary procedure of external ventricular drain.
After definitive surgery like VP shunt, we don’t remove the reservoir till there is complication. It acts as a gateway in the event of acute shunt obstruction and also it can help in plotting intracranial pressure in suspicious case of under working shunt.
Chosen site of ommaya reservoir implantation is Kocher’s point, but in neonates we usually choose a bony area over right frontal horn so reservoir has a bony support to prevent it from sinking. Adequate subcutaneous tunneling must be done to accommodate CSF while pressure rises. Incision should be away from reservoir and never be over it. Catheter length is maintained exactly the same measurement of cranial end of shunt. We usually tap the catheter, after palpating fontanelle for fullness with help of 25 G butterfly needle maintaining all aseptic precaution and approximately 10-15 ml/kg CSF is aspirated per tap [23,24].
The frequency of tapping were considered to be adequate if increase in head circumference is less than 1 cm/week, normal tension of the fontanelle and normal position of the cranial sutures. Following CSF aspiration all cases were administered vancomycin 15 to 20 mg as IVT. In all patients’ normal increase in OFC, decrease of OFC who had enlarged head, normal tension of fontanelle and normal position of suture were achieved. The following complications were kept in mind regarding doing it. Those were infection of reservoir (positive CSF culture), breakdown of overlying skin, intra ventricular hemorrhage and obstruction of the catheter, newly found seizure attack [25]. Data analysis was done by statistical software SPSS version [26].
Results
During the study period, n=33 consecutive cases of reservoir implantation were taken into the study irrespective of etiology of hydrocephalus (Table 1).
| Mode of presentation | Number | Percentage |
|---|---|---|
| Infantile hydrocephalus | 28 | 84.84% |
| Ventriculitis following reservoir infection | 3 | 9% |
| Ventriculitis following shunt infection | 2 | 6.06% |
Table 1: According to mode of presentation.
28 patients presented with infantile hydrocephalus. All of them underwent ETV along with reservoir implantation.
3 patients presented with ventriculitis following reservoir implantation and another 2 with infected V-P shunt. Those were referred to our institution from Government medical institutions. The foreign body was immediately removed followed by EVD (External Ventricular Drain) insertion. Infection was controlled by appropriate parenteral and IVT where feasible.
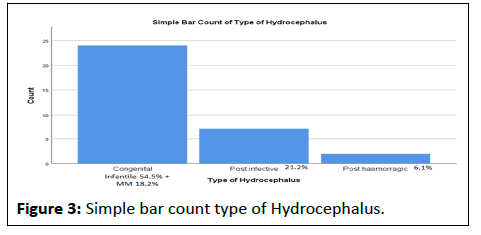
After correction of infection we implanted a new reservoir in another site (Figure 3).
Among the types of hydrocephalus, congenital and meningomyelocele group was predominant. Most of the mothers (91.7%) of congenital and MM group had folic acid after 2 months of pregnancy i.e. after formation of neural tube.
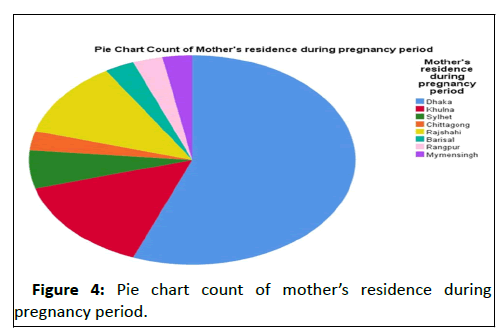
Low socioeconomic status significantly associated with low body weight at presentation (p=0.007). Besides most of the congenital and MM group (48.48%) belonged to low socioeconomic group (Figure 4).
Vast majority of the affected babies mother had their periconceptional periodi n arsenic belt and area of rapid industrialization in Bangladesh (Table 2).
| Age at reservoir placement (days) | Average volume aspirated | CSF aspiration per week | First complication with reservoir | First complication days after reservoir placement | Subsequent complication | Re intervention |
|---|---|---|---|---|---|---|
| 90 | 40cc | 3 times | Subcutaneous CSF
leak f/by skin sloughedout |
25 days | No | EVD
f/V-P shunt |
| 35 | 15cc | 3 times | Ventriculitis | 5 days | No | EVD
f/Ommayareplacement |
| 337 | 80cc | 3 times | Cutaneous inflammation+ Ventriculitis | 210
days |
No | EVD
f/Ommayareplacement |
Table 2: Details of the three patients having reservoir complications in our institution.
Majority of the patients (42.4%) had CSF aspiration two times weekly with an average volume of 20-50 ml per aspiration (54.5%). Following CSF aspiration all cases were administered vancomycin 15 to 20 mg as IVT.
No intraoperative complications had occurred among all the cases. Later complications had occurred in 3 babies (9.1%). Table 2 showing details of the 3 patients with complications. One was a preterm, 900 gm infant suffered with Pseudomonas related ventriculitis who initially had PHH. Wound dehiscence occurred in one case that developed ETV failure and presented late. Next baby was a case of bilateral shunt infection with torch positive with features of emaciation. He developed late reservoir complication as a result of cushing syndrome. He had been treated with ACTH for intractable convulsion (Table 3).
| ETV+Ommaya reservoir implantation | 23 (69.7%) |
| Ommaya reservoir implantation | 5 (15.15%) |
| EVD (External Ventricular Drain) | 5 (15.15%) |
Table 3: Primary surgery done in BMCH.
ETV along with reservoir implantation was done in 69.7% of patients. Few cases (15.15%) only Ommaya reservoir implantation was done as babies were not fit for general anesthesia and rest (15.15%) had EVD as primary surgery as they presented with ventriculitis following infected VP shunt or reservoir implantation done elsewhere.
2 babies had died 1 year after reservoir implantation due to unrelated disease. Out of the 31 survivors, 3 patients did not need any further aspiration and 19 patients needed v-p shunt, but reservoir was kept in situ for future emergency. Rest of them is waiting for definitive VP shunt procedure.
36.4% babies have reservoir in their body for more than 1 year with or without VP shunt. There was no definitive relationship between duration of reservoir in body and reservoir complication. No surviving patient was lost at follow up.
Discussion
In our practice, we observed VP Shunt infection mostly occurs in premature, infants less than 6 months and low birth weight babies with thin skin. So, we follow the system to delay shunt and we advocate ETV+reservoir implantation is the treatment of choice in any infants with hydrocephalus. In this study we didn’t include the post tumoral hydrocephalus group as most of them were referred to other hospital and contacts were lost. But we found the palliative role of ommaya reservoir where the tumor was inoperable and repeated shunt blockage due to high protein content of CSF.
Treatment of pre term and low birth weight hydrocephalic infant is a major challenge. Though we do ETV, there is possibility of ETV failure at very early and late cases. Moreover, the baby may be in remote place in the event of failure. If a reservoir was placed in the ETV port it could be managed.
In case of premature infants with hydrocephalus, Ventriculoperitonal Shunt (VPS) is the final treatment of choice for CSF diversion. However, some patients need temporary bypass of the normal CSF pathways while awaiting improvement of liquor characteristics, abdominal status, or local or systemic infections. Ommaya reservoir plays the most crucial role in delaying shunt.
Ramin Eshkandari and his team worked with kaolin induced animal model of hydrocephalus concluded tapping of reservoir in neonatal hydrocephalus based on neurological deficit. This procedure does not halt progressive ventricular enlargement and there is definite correlation between neurological deficit and ventricular enlargement [26].
Though this study did not have this component of study but there is space for future study regarding neuro development of these babies.
Romergryko, et al. demonstrated continuous ICP monitoring is able to identify larger number of shunt malfunction [27]. In our institution we use chhabra shunt as it got a very good tolerance, inexpensive. So here ommaya reservoir remains as a golden gate which can provide ICP monitoring in future malfunction.
N. Bruinisma and team carried out a retrospective study regarding subcutaneous ventricular catheter reservoir and ventricle peritoneal drain related infections. They concluded prematurity, extreme low birth weight is more prone to infection [28]. In our study, one pre term with extreme low birth weight neonate had cerebral catheter related ventriculitis, which was treated successfully.
A Leonhardt and team used ventricular reservoir for treatment of post hemorrhagic hydrocephalus. They found there was no serious complication except skin breakdown [29].
We usually don’t advocate shunt in those neonates in event of ETV failure until they are 4 months and gain the ideal weight for this age. Placement of Ommaya Reservoir gives us ample time to gain weight and delaying shunt.
Sarah J Gaskill, et al. included 38 preterm babies of NICU with severe respiratory distress syndrome having PHH. They found reservoir implantation is a logical and benign solution to this difficult problem. The majority of the reservoirs were left in place for 1-2 months. There was no reservoir infection [30].
In our study, we included hydrocephalus of all etiology except the post tumoral and post head injury type. There were only 2 cases of PHH, among them one baby had ventriculitis by Pseudomonas. She was treated by EVD. Parenteral and intraventricular colomycin was administered for 14 days subsequently. At that time she weighted only 900 gm and 29 weeks of gestation. She had VP shunt (Y type) at the age of 4 months and caught up all developmental milestones till date.
Bangladesh is a third world country and our hospital is working for the poorest. We use chhabra medium pressure shunt which seems to be very effective. We do ETV+reservoir implantation as the first surgery in any neonatal hydrocephalus. If ETV fails after short time, CSF is regularly aspirated till they achieve sufficient weight to comply with shunt. We found 2 cases of very late ETV failure nearly after 8 years and both lost their eyesight. Idea of implantation of Ommaya reservoir arose from it. It can be very effective in diagnosing sub optimally working ETV. Miljan Milhajlovic and team had a paper on treatment modalities of post hemorrhagic hydrocephalus in prematurely born children and found predictors of poor outcome of ommaya reservoir implantation are low birth weight, low apgar score, presence of extended assisted ventilation in extended period, peripheral asphyxia and cardio respiratory arrest [31]. As N. Bruinisma and colleague concluded we maintained strict skin preparation by chlorhexidine and prophylactic intra thecal vancomycin (15-20 mg) after each tapping. Children who develop hydrocephalus secondary to intraventricular hemorrhage are more susceptible to develop shunt infections as they have congenital immune deficiency.
That’s why early shunt placement for post hemorrhagic hydrocephalus is mostly ineffective and associated with an increased risk of infection. In a study with 19 premature infants who had post hemorrhagic HCP and had undergone early VP shunt, revealed a shunt infection rate of approximately 21%.
Temporary measures, such as extra ventricular drainage or ventricular tapping, may be undertaken until the patient tolerance increases [32]. Mc Girt, et al. reported there was a fourfold increase in risk of shunt infection those who had previous shunt infection and Kestle, et al. observed a 30% rate of infection recurrence [33,34]. Sciubba, et al. reported that V-P shunt placement in premature neonates was associated with approximately five-fold increase in the risk of shunt infections. A retrospective review by Vinchon, et al. on the occurrence of shunt infections in premature neonates evoked the proposed recommendation that ventricular taps and external ventricular drainage in these children are effective until they become fit for the definitive VP shunt procedure [35,36]. Maitrey, et al. found a definitive relationship between arsenic and folate deficiency leading to neural tube defects [37]. On our limited study, most of the mothers of spine bifida and congenital hydrocephalus group spend their initial part of pregnancy in arsenic zone of Bangladesh. Moreover, those parents were from where rapid urbanization was going on and environmental air had high lead content. Talip Karacor, et al. showed lead level was statistically high in the neural tube defect group. It calls for further study in Bangladesh to see if environmental lead has any effect on genesis of the disease process. Here, external ventricular drainage was given in cases of infected shunts in emaciated babies. In those cases after removal of EVD, Ommaya reservoir was placed for regular tapping till they achieve sufficient weight.
Conclusion
Ommaya reservoir is extremely effective in delaying shunt ins ertion. Its complication rate is low and got various usages. CSF aspiration through ommaya reservoir is easy and this method has got very good prospective in low birth weight and emaciated cases of hydrocephalus.
References
- Rekate HL (2008) The definition and classification of hydrocephalus: a personal recommendation to stimulate debate. Cerebrospinal Fluid Res 5:1-7
[Crossref] [Googlescholar][Indexed]
- Kaye AH (2005) Essential Neurosurgery. (3rd edition). Blackwell Publishing Ltd, Massachusetts, USA, 31-36
- Rocco Di, Cinalli CG, Maixner WJ, Sainte-Rose C (2006) Pediatric hydrocephalus. Childs Nerv Syst 22:204-205
- Goel AK, Pandya SK (1996) Hydrochephalus, in Text Book of Neurosurgery. 2nd edition. BI Churchill Livingstone Pvt. Ltd. New Delhi, India 195-216
- Hintz SR, Poole WK, Wright LL, Fanaroff AA, Kendrick DE, et al. (2005) Changes in mortality and morbidities among infants born at less than 25 weeks during the post surfactant era. Arch Dis Child Fetal Neonatal Ed 90:128-133
[Crossref] [Googlescholar] [Indexed]
- Rahman MM, Haque MA, Islam MR, Salam MA, Uddin K, et al. (2015) Demographic characteristics and etiology of hydrocephalus patients attended at tertiary care hospital in Bangladesh. J Natl Inst Neurosci Bangladesh 1:47-49
- Mihajlovic M, Bogosavljevic V, Nikolic I, Mrdak M, Repac N (2013) Surgical treatment problems of hydrocephalus caused by spontaneus intraventricular hemorrhage in prematurely born children. Turk Neurosurg 23:593-599
- Lee JK, Seok JY, Lee JH, Choi EH, Phi JH, et al. (2012) Incidence and risk factors of ventriculoperitoneal shunt infections in children: a study of 333 consecutive shunts in 6 years. J Kor Med Sci 27:1563-1568
- Renier D, Lacombe J, Pierre-Kahn A, Sainte-Rose C, Hirsch JF (1984) Factors causing acute shunt infection: computer analysis of 1174 operations. J Neurosurg 61:1072-1078
- Choux M, Genitori L, Lang D, Lena G (1992) Shunt implantation: reducing the incidence of shunt infection. J Neurosurg 77:875-880
[Crossref] [Googlescholar] [Indexed]
- Pople IK, Bayston R, Hayward RD (1992) Infection of cerebrospinal fluid shunts in infants: a study of etiological factors. J Neurosurg 77:29-36
[Crossref] [Googlescholar] [Indexed]
- Mancao M, Miller C, Cochrane B, Hoff C, Sauter K, et al. (1998) Cerebrospinal fluid shunt infections in infants and children in Mobile, Alabama. Acta Paediatr 87:667-670
- Kulkarni AV, Drake JM, Lamberti-Pasculli M (2001) Cerebrospinal fluid shunt infection: a prospective study of risk factors. J Neurosurg 94:195-201
[Crossref] [Googlescholar][Indexed]
- Kulkarni AV, Rabin D, Lamberti-Pasculli M, Drake JM (2001) Repeat cerebrospinal fluid shunt infection in children. Pediatr Neurosurg 35:66-71
- Gaskill SJ, Martin AE, Rivera S (1988) The subcutaneous ventricular reservoir: an effective treatment for posthemorrhagic hydrocephalus. Child Nerv Syst 4:291-295
- McComb JG, Ramos AD, Platzker AC, Henderson DJ, Segall HD (1983) Management of hydrocephalus secondary to intraventriculare hemorrhage in preterm infant with subcutaneous ventricular catheter reservoir. Neurosurg 13:295-300
- Richard E, Cinalli G, Assis D, Pierre-Kahn A, Lacaze-Masmonteil T (2001) Treatment of post haemorrhage ventricular dilatation with an Ommaya’s reservoir: Management and outcome of 64 preterm infants. Childs Nerv Syst 17:334-340
- Peretta P, Ragazzi P, Carlino CF, Gaglini P, Cinalli G (2007) The role of Ommaya reservoir and endoscopic third ventriculostomy in the management of post-hemorrhagic hydrocephalus of prematurity. Child Nerv Syst 23:765-771
- Das S, Rahman A, Nath HD, Halder R, Ghosh D (2021) Thirty days complications of pediatric hydrocephalus following ventriculoperitoneal shunt surgery. Int J Neurol 10:8-33
- Sabeti M, Boostani R, Moradi E, Habibi Z, Nejat F (2021) Predicting shunt infection in children with hydrocephalus. Intell Med 5:100029
- Peretta P, Ragazzi P, Carlino CF, Gaglini P, Cinalli G (2007) The role of Ommaya reservoir and endoscopic third ventriculostomy in the management of post hemorrhagic hydrocephalus of prematurity. Childs Nerv Syst 23:765-771
[Crossref] [Googlescholar ][Indexed]
- Geocadin RG, Varelas PN, Rigamonti D, Williams MA (2007) Continuous intracranial pressure monitoring via the shunt reservoir to assess suspected shunt malfunction in adults with hydrocephalus. Neurosurg Focus 22:1-6
[Crossref] [Googlescholar][Indexed]
- Flores AP, Gutiérrez JS, Reyes JR, Tamayo JS, Benito FC (2020) Risk factors associated with conversion of an Ommaya reservoir to a permanent cerebrospinal fluid shunt in preterm post hemorrhagic hydrocephalus. J Neurosurg: Pediatrics 25:417-424
- Leonhardt A, Steiner HH, Linderkamp O (1989) Management of posthaemorrhagic hydrocephalus with a subcutaneous ventricular catheter reservoir in premature infants. Arch Dis Child 64:24-28
- Eskandari R, Packer M, Burdett EC, McAllister JP (2012) Effect of delayed intermittent ventricular drainage on ventriculomegaly and neurological deficits in experimental neonatal hydrocephalus. Childs Nerv Syst 28:1849-1861
- Geocadin RG, Varelas PN, Rigamonti D, Williams MA (2007) Continuous intracranial pressure monitoring via the shunt reservoir to assess suspected shunt malfunction in adults with hydrocephalus. Neurosurg Focus 22:1-6
[Crossref] [Googlescholar][Indexed]
- Bruinsma N, Stobberingh EE, Herpers MJHM, Vles JSH, Weber BJ, et al. (2000) Subcutaneous ventricular catheter reservoir and ventriculoperitoneal drain-related infections in preterm infants and young children. Clin Microbiol Infect 6:202-206
- Leonhardt A, Steiner HH, Linderkamp O (1989) Management of posthaemorrhagic hydrocephalus with a subcutaneous ventricular catheter reservoir in premature infants. Arch Dis Child 64:24-28
- Gaskill SJ, Marlin AE, Rivera S (1988) The subcutaneous ventricular reservoir: an effective treatment for posthemorrhagic hydrocephalus. Childs Nerv Syst 4:291–295
- Mihajlovic M, Mrdak M, Radlovic V, Nikolic I, Rakic M, et al. (2013) Application of the Ommaya reservoir in the treatment of hydrocephalus in prematurely born children: correlation with animal results. Srpski arhiv za celokupno lekarstvo 141:8-12
- Ahn SY, Shim SY, Sung IK (205) Intraventricular hemorrhage and post hemorrhagic hydrocephalus among very low birth weight infants in Korea. J Korean Med Sci 30:52-58
- McGirt MJ, Zaas A, Fuchs HE, George TM, Kaye K, et al. (2003) Risk factors for pediatric ventriculoperitoneal shunt infection and predictors of infectious pathogens. Clin Infect Dis 36:858-862
- Kestle JR, Hoffman HJ, Soloniuk D, Humphreys RP, Drake JM, et al. (1993) A concerted effort to prevent shunt infection. Childs Nerv Syst 9:163-165
[Crossref] [Googlescholar][Indexed]
- Sciubba DM, Noggle JC, Carson BS, Jallo GI (2008) Antibiotic impregnated shunt catheters for the treatment of infantile hydrocephalus. Pediatr Neurosurg 44:91-96
- Vinchon M, Baroncini M, Laurent T, Patrick D (2006) Bowel perforation caused by peritoneal shunt catheters: diagnosis and treatment. Neurosurgery 58:76-82
- Mazumdar M, Ibne Hasan MOS, Hamid R, Valeri L, Paul L, et al. (2015) Arsenic is associated with reduced effect of folic acid in myelomeningocele prevention: a case control study in Bangladesh. Environ Health 14:1-8
- Karacor T, Kirici P, Nacar MC, Bulbul M, Onderci M, et al. (2020) Evaluation of specific heavy metal levels of pregnant women complicated by neural tube defects. Ann Med Res 27:460
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences