Pearls on Child Skin
Sharanya K and Narasimhalu CRV
DOI10.21767/2573-0282.100028
Sharanya K and Narasimhalu CRV*
Venereology and Leprosy, Department of Dermatology, Saveetha Medical College, Saveetha University, Thandalam, Chennai, Tamil Nadu, India
- *Corresponding Author:
- Narasimhalu CRV
Venereology and Leprosy, Department of Dermatology
Saveetha Medical College, Saveetha University
Thandalam, Chennai, Tamil Nadu, India
Tel: +91-9790718424
E-mail: drnarasimhalu@yahoo.co.in
Received date: September 24, 2016; Accepted date: October 14, 2016; Published date: October 17, 2016
Citation: Sharanya K , Narasimhalu CRV (2016) Pearls on Child Skin. Pediatric Infect Dis 1:28. doi: 10.21767/2573-0282.100028
Keywords
Molluscum contagiosum; Virus disease; Waxy papules; Pox virus
Introduction
Molluscum Contagiosum (MC) is a common, self-limiting viral disease of skin and mucous membrane, caused by Molluscum Contagiosum virus (MCV 1-4), which is DNA virus belonging to poxvirus family. MC is common infection in children between ages 1-12 years. It is also seen in sexually active adults and those who are immunocompromised. Clinically MC appears as small bumps, which are called as “Mollusca” on the skin or mucous membrane.
Case Report
A 6 year old male child referred to our outpatient department with multiple skins colored raised lesions over the left side of face for the past 2 months. Initially it started as a single small sized skin colored raised lesion and later it increased in size and number and attained the present size. Lesions were not associated with any pain or discomfort. There was no history of frequent infection. No history of malnutrition or nutritional deficiencies was detected. No history of similar lesions was detected in his family.
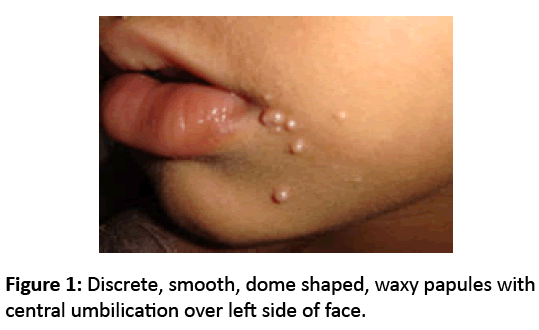
Dermatological examination showed multiple discrete, smooth, dome shaped, waxy papule with central umbilication, size ranging from 0.5-1.0 cm, distributed on face particularly on left side of mouth (Figure 1). Routine blood investigations revealed no abnormality. The diagnosis of molluscum contagiosum was made on basis of history and clinical examination [1-3].
Discussion
Molluscum Contagiosum is a superficial, viral infection, which is characterized by single, discrete or multiple popular or nodular lesions on skin or mucous membrane. Molluscum Contagiosum was first described by Bateman in 1817. In 1841, Henderson and Peterson described the intracytoplasmic inclusion bodies now known as molluscum or Henderson- Peterson bodies. In 1905, Juliusburg proved its viral nature [1].
Molluscum Contagiosum virus is transmitted directly by skin contact to produce the typical cutaneous and rarely mucosal lesion. Transmission via fomites on bath sponges and bath towels, school swimming pools and Turkish baths have been implicated as source of infection [2,3]. The incubation period usually varies from 14 days to 6 months [4]. Typically, molluscum lesion begins as painless, small papules, which later becomes raised to pearly, flesh colored, dome shaped papules or nodules with a central depression like small pit or umbilication. The central pit contains central plug of waxy, cheesy, white material in which virus is present. The lesion may be solitary or multiple and they measure about 2-5 mm and sometimes grow too large as 10 mm [5]. Most patients develop multiple papules in intertriginous sites, such as axilla, popliteal fossa and groin [6]. Lesions often appear in clusters or in linear pattern. The latter often result from koebnerization [7]. Diagnosis of lesion is usually based on clinical findings. A histopathological assessment is required in atypical variant cases.
MC lesions spontaneously resolve when left untreated within 6-18 months in children and immuno-competent adults. Treatment is recommended for cosmetic reason and to prevent autoinoculation, based on patient’s age, immune status and site of lesion.
Many topical agents can be used to produce mild to moderate inflammation and hence potentially stimulate the development of an immune response against the virus. Cantharidin, trichloroacetic acid and diluted liquefied phenol are strong irritants which can both cause pain, blistering and scarring but with careful application and appropriate dilution can increase lesion clearance [8-10]. Surgical removal of molluscum contagiosum by curettage has been used for many years. Children will usually need prior application of topical anaesthetic cream with strict observance of the maximum safe dose [11]. Cryotherapy is effective and commonly used in older children and adults, but needs to be repeated at 3-4 weekly intervals. Photodynamic therapy has also been used with effect [12].
References
- Hanson D, Diven DG (2003) Molluscumcontagiosum. Dermatol online J 9:2.
- Niizeki k, Kano O, Yoshiro K (1984) An epidemic study of mollusucumcontagiosum: Relationship to swimming pools:an epidemiologic study[letter]. Dermatolo 191: 165.
- Choong KY, Roberts LJ(1999) Molluscumcontagiosum, swimming and bathing: a clinical analysis. Australs J Dermatol 40:89-92.
- Sterling JC (2004) VIRUS INFECTIONS. In: Burns T, Breathnach S, Cox N, Griffith C (eds.).Rook’s Textbook of dermatology.7thedn. London: Balckwell Publishing company 25: 11-25.
- Nandhini G. Rajkumar K, Kanth KS, Nataraj P, Ananthakrishnan P, (2015) Molluscumcontagiosum in a 12 year old child-Report of a case and review of literature. J Int Oral Health 7:63-66.
- Tom W, Friedlander SF (2008) Poxvirus infections. In: Fitzpatrick TB, Freedberg IM, Eison AZ, Wolff K, Austenk F, Goldsmith LA, Katz SI(eds.). Fitzpatrick’s Dermatology in general medicine. 6 thedn. New york, McGraw Hill-company 34: 1081.
- Brown J, Janniger CK, Schwartz RA, Silverberg NB (2006) Childhood molluscumcontagiosum. Int J Dermatol 45:93-99.
- Weller R, Callaghan CJ, MacSween RM (1999) Scarring in Molluscumcontagiosum: comparison of physical expression and phenol ablation. BMJ 319:1540.
- Silverberg NB, Sidbury R, Mancini AJ (2000) Childhood molluscumcontagiosum:experience with cantharidin therapy in 300 patients. J Am AcadDermatol 43: 503-507.
- Garrett SJ, Robinson JK, Roenigk HH (1992)Trichloroacetic acid peel of Molluscumcontagiosum in immunocompromised patients. J DermatolSurgOncol 18:855-858.
- Rönnerfält L, Fransson J, Wahlgren CF (1998) EMLA cream provides rapid pain relief for the curettage of molluscumcontagiosum in children with atopic dermatitis without causing serious application-site reactions. PediatrDermatol 15:309-312.
- Gold MH, Moiin A (2007) Treatment of verrucae vulgaris and molluscumcontagiosum with photodynamic therapy. DermatolClin 25: 75-80.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences