Paediatric Mastoid Subperiosteal Abscess: Diagnostic and Treatment Essentials
Charalampos Voudouris, Ioannis M. Psarommatis
DOI10.21767/2573-0282.100021
Charalampos Voudouris* and Ioannis M. Psarommatis
Department of ENT, "P. & A. Kyriakou" Children’s Hospital of Athens, Greece
- *Corresponding Author:
- Charalampos Voudouris
Department of ENT
"P. & A. Kyriakou" Children’s Hospital of Athens
Athens, Greece
E-mail: xvoudouris@hotmail.com
Received date: July 04, 2016; Accepted date: August 08, 2016; Published date: August 12, 2016
Citation: Voudouris C, Psarommatis IM (2016) Paediatric Mastoid Subperiosteal Abscess: Diagnostic and Treatment Essentials. Pediatric Infect Dis 1:21. doi: 10.21767/2573-0282.100021
Abstract
Mastoid subperiosteal abscess (SA) is the most common complication of acute mastoiditis. Today, no uniformly accepted diagnostic or treatment protocols exist. Imaging studies for all patients and mastoidectomy plus myringotomy, traditionally constitute the gold-standard of treatment methods. However, more conservative approaches viewed as safe and reliable alternative options for the clinician have recently gained popularity. In this review authors try to answer some vital questions regarding the diagnosis and management of SA in children, based on the relevant literature and their personal experience.
Keywords
Acute mastoiditis, Subperiosteal abscess, Children
Abbreviations
CT: Computed Tomography; ENT: Ear, Nose and Throat; MRI: Magnetic Resonance Imaging; MRV: Magneting Resonance Venography; SA: Subperiosteal Abscess.
Introduction
Mastoid subperiosteal abscess is the most common complication of acute mastoiditis, classified in the spectrum of intratemporal complications of acute otitis media. The classic sequence of SA formation is the extrusion of pus beneath the periosteum through infectious erosion of the outer cortical bone at the mastoid protuberance or through pre-existing anatomical pathways, such as vascular channels and the tympano-mastoid suture [1,2].
All researchers agree that parenteral antibiotics are paramount for patients suffering from acute mastoiditis with or without SA formation. However, in terms of surgical treatment strategies, intense controversies and definitely no universally accepted treatment protocols- so far exist.
SA has always been regarded as a surgical entity, with mastoidectomy plus myringotomy traditionally constituting the gold-standard of treatment methods [3-5]. Recently, conservative surgical measures, involving myringotomy plus incisional drainage or needle aspiration of the abscess, have also been adopted by many authors [6-9]. Simple mastoidectomy is thus preserved for poor responders or for those presenting associated cholosteatoma or intracranial complications.
This work is not an extensive review of the bibliography about the SA in children. Instead, it aims at answering practical key-questions on the topic and attempts to come up with a treatment algorithm for SA, mainly based on the clinical experience gained in a tertiary pediatric center.
Questioning
How is the diagnosis being set?
The diagnostic process of SA is mainly based on clinical examination. The clinical diagnostic criteria are those of acute mastoiditis, which consist of recent history of acute otitis media, retroauricular inflammatory redness/swelling/pain and antero-inferior protrusion of the auricle, combined with retroauricular fluctuation and/or bulging of the posterosuperior wall of the external auditory canal.
Pus aspiration in cases of SA plays an important role in diagnosis. This method has the disadvantage of requiring general anesthesia, but can practically be applied in all cases of acute mastoiditis, following myringotomy. Doing so, we were able to diagnose SAs in cases of acute mastoiditis without palpable postauricular fluctuation or posterior canal wall bulging, which otherwise would have remained undiagnosed.
The diagnosis of SA can be enhanced by imaging findings but according to our approach a temporal bone CT scan just to make the diagnosis of SA is not recommended. Definitively, diagnosis is confirmed or rejected during surgery.
In which cases could imaging studies be avoided?
Βrain irradiation caused by the extensive use of CT scans in the pediatric population and its possible long-term consequences, have always been raising radiation protection concerns among researchers [6-8].
Although routine use of CT scanning is proposed by many authors [9-13], it is our firm belief that in typical cases of SA with an obvious clinical diagnosis, CT scans may possibly be withheld. Nevertheless, attending physicians should be equipped with a low threshold for ordering the appropriate imaging study.
n cases of mastoid subperiosteal abscess, preoperative imaging is considered mandatory in:
• suspected intracranial complications
• underlying cholosteatoma
• recurrent mastoiditis
• "Atypical" presentation, when diagnosis is in doubt.
CT or MRI is the best imaging choice?
CT scan protocols for the complications of acute otitis media include high resolution temporal bones scan without contrast and contrast-enhanced brain CT. Unenhanced temporal bones CT scans are suitable for identifying suspected cholosteatomas, and delineating bony architecture. However, if a suspected intracranial complication (e.g cerebral/epidural/ subdural abscess, sigmoid sinus thrombosis) is the case, a contrast-enhanced brain CT scan or MRI are more appropriate options [12,14].
Albeit less available, more time consuming and more expensive, MRI (including MRV) does not involve ionizing radiation exposure and is considered the "gold standard" method for uncovering acute mastoiditis-related intracranial complications [12].
In cases where brain CT scans are either inconclusive or negative but intracranial complications are still suspected, an MRI scan should be obtained, as even subtle intracranial abnormalities, which may remain invisible on CT, can be demonstrated on the MRI [12,14].
Empiric intravenous antibiotic protocols: monotherapy or combinations?
The choice of an appropriate empiric antibiotic treatment and its initiation shortly after admission -long before sensitivity test results are usually available and targeted antibiotic treatment possible- is of paramount significance for a positive clinical outcome. The antibiotic therapy scheme in our published series included a third generation cephalosporin (cefotaxime or ceftriaxone) plus clindamycin, coveringtheoretically- almost the whole spectrum of micro-organisms known to be involved in acute mastoiditis. Although monotherapy is effective in most cases, always leaves a higher possibility of microbial growth, potentially exposing the patients to the toxicity of the responsible microorganism. To our experience and based on the current level of knowledge on the subject, combined antibiotic therapy is a safer option for patients than monotherapy, without necessarily showing more adverse effects or higher costs [15].
What does conservative surgical management of subperiosteal abscess entail?
Conservative surgical management of SA comprises myringotomy and drainage of the abscess, via incision or needle aspiration.
The utilization of incisional myringotomy with or without ventilation tube insertion, laser myringotomy, as well as widefield myringotomy (inferior-posterior quadrant of the tympanic membrane) have all been reported in literature [6,9], with the latter being the author’s preference for all children suffering from SA, including those presenting otorrhea.
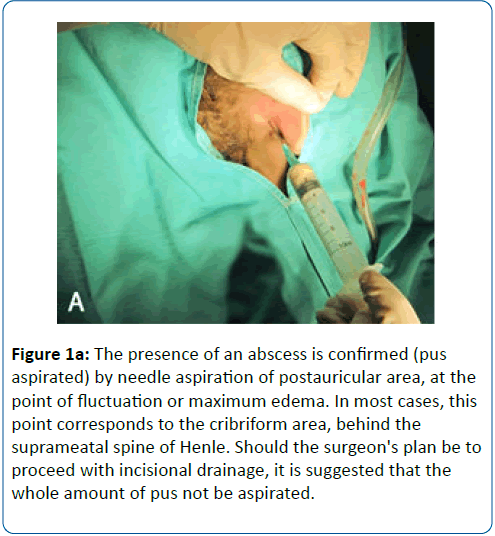
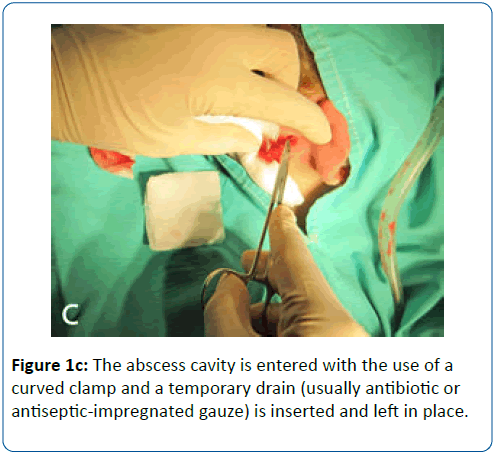
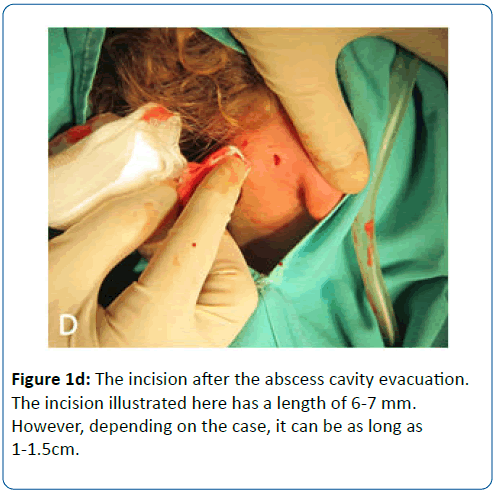
Concerning the abscess drainage, a needle and syringe can be of great aid for confirmation and localization. After having confirmed the existence of abscess (pus aspiration), the surgeon has two options: a) emptying the abscess with the aspiration needle and b) draining the abscess by incision. The second option is showed in Figures 1a-1d.
Figure 1A: The presence of an abscess is confirmed (pus aspirated) by needle aspiration of postauricular area, at the point of fluctuation or maximum edema. In most cases, this point corresponds to the cribriform area, behind the suprameatal spine of Henle. Should the surgeon's plan be to proceed with incisional drainage, it is suggested that the whole amount of pus not be aspirated.
Specimens of pus should be obtained in all cases from the middle ear (during myringotomy) and form the abscess cavity for culture and sensitivity testing.
Conservative surgery or mastoidectomy?
Mastoidectomy remains the most reliable and effective procedure for acute mastoiditis and subperiosteal abscess definite treatment, with low treatment failure rates. In our series, all patients treated with simple mastoidectomy were cured without any complications, having an uneventful postoperative period [16].
Meanwhile, conservative surgery has been found to be a safe and reliable first-line treatment method. Based on its advantages and disadvantages -which are summarized on Table 1 conservative surgical approach can be credited for first line treatment of SA in children but one should be prepared to perform simple mastoidectomy in children showing poor response.
| Advantages | Disadvantages |
|---|---|
| Safe (if combined with myringotomy and IV antibiotics). | Not always effective: children failing to respond should be subjected to simple mastoidectomy. |
| Quick and simple to perform. | Initial treatment failure and subsequent application of simple mastoidectomy may prolong hospitalization by 2-3 days. |
| Short general anaesthesia duration. | |
| Practically no intraoperative risks. | |
| Minimal blood loss. | |
| Low cost. | |
| Shorter duration of hospitalization compared to mastoidectomized children. | |
| Lack of postoperative complications. | |
| Preservation of mastoidectomy for treatment failure salvage. |
Table 1: Advantages and disadvantages of conservative surgical management of mastoid subperiosteal abscess in children.
How much "conservative" is safe?
Many researchers endorse conservative surgical management of SA in children as a safe and efficient method. Bakhos et al reported only one failure among 16 cases of conservative management, which was successfully treated with cortical mastoidectomy [9], while Enokson et al. found minor surgical treatment sufficient in 32 out of 33 cases, in a retrospective multicenter study [17]. According to our experience, however, about half of the children with subperiosteal abscess will be successfully treated using conservative surgical approach whereas the remaining will be subjected to mastoidectomy.
Diverging from the view of some pediatric centers applying conservative surgical management even in cases suffering from otogenic intracranial complications [18-20] we consider that strict rules and a minimum of pre-requisites should be rigorously followed in favour of children's safety:
• Not all children are candidates for conservative surgical treatment. Children with suspected cholosteatoma as well as those suffering from intracranial suppurative complications should be treated with mastoidectomy in all cases of acute mastoiditis, with or without subperiosteal abscess.
• First-line conservative surgical treatment and initiation of intravenous antibiotics within hours after admission contribute to a favourable therapeutic result.
• Clinical and laboratory criteria should be applied and decisively followed for patient re-evaluation, 48-72 hours after admission. These criteria should include auricular displacement restoration AND recovery of retroauricular local signs AND decreasing values of non-specific inflammatory markers AND fever fading (if any).
• Unresponsive cases (failure to improve or deterioration of clinical and/or laboratory findings) ought to be treated with simple mastoidectomy within few days after admission, avoiding repeat myringotomies or abscess drainages.
When is ENT consultation necessary?
In all cases. SA forms a disease that positively requires surgical measures -among others- to be safely treated either minor or major ones. ENT consultation is recommended even in cases with suspected SA. Apart from SAs, it is our belief that an ENT evaluation is also needed in all cases of pediatric acute mastoiditis -the "mother disease", either complicated or not. This attitude arises from the likelihood of developing severe/ lethal complications in cases with delayed diagnosis or inappropriate management. Although this possibility may be small, it should be eliminated completely.
Algorithmic approach
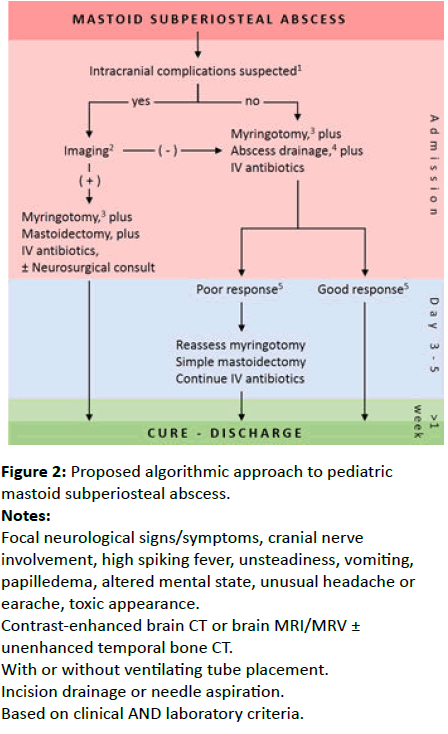
A standardized protocol to pediatric SA might facilitate greatly its management. This can also be a substantial help for less experienced physicians. The algorithm shown in Figure 2 represents the accumulated experience on the subject in our tertiary pediatric center.
Figure 2: Proposed algorithmic approach to pediatric mastoid subperiosteal abscess; Notes: Focal neurological signs/symptoms, cranial nerve involvement, high spiking fever, unsteadiness, vomiting, papilledema, altered mental state, unusual headache or earache, toxic appearance; Contrast-enhanced brain CT or brain MRI/MRV ± unenhanced temporal bone CT; With or without ventilating tube placement; Incision drainage or needle aspiration; Based on clinical AND laboratory criteria.
In the typical case of a pediatric SA with an obvious clinical diagnosis and without additional complications suspected, combined intravenous antibiotic therapy and conservative surgical measures are suggested within hours after admission. The child is monitored closely and continuously, and the critical re-evaluation takes place 48-72 hours after the initiation of therapy. In cases of good response, no further surgical treatment is required and patients can safely be discharged usually in 8-10 days. Poor responders should undergo simple mastoidectomy within 3-5 days after admission. In cases with suspected intracranial complications, imaging studies should be performed without delay. Patients proved free of further complications on imaging are potential candidates for conservative surgical approach. In cases in which SA is combined with an intracranial complication, myringotomy and mastoidectomy should follow as soon as possible and preferably in neurologically stable children. In such cases, neurosurgical consultation and assistance at operating room may be necessary [18-20].
References
- Budenz C, El-Kashlan H, Shelton C, Aygun N, Niparko J (2015) Complications of Temporal Bone Infections. Cummings Otolaryngology Head and Neck Surgery 6th edn. Philadelphia: Saunders-Elsevier pp: 2156-2176.
- Migirov L, Yakirevitch A, Kronenberg J (2005) Mastoid subperiosteal abscess: a review of 51 cases. Int J PeditrOtorhinolaryngol 69: 1529-1533.
- Gliklich RE, Eavey RD, Iannuzzi RA, Camacho AE (1996) A contemporary analysis of acute mastoiditis. Arch Otolaryngol Head Neck Surg 122: 135-94.
- Goldstein NA, Casselbrant ML, Bluestone CD, Kurs-Lasky M (1998) Intratemporal complications of acute otitis media in infants and children. Otolaryngol Head Neck Surg 119: 444-454.
- Neely JG (2010) Surgery of acute infections and their complications. In: Brackmann DE, Shelton C, Arriaga MA, editors. Otologic Surgery 3rd edn. Philadelphia: Saunders-Elsevier. pp: 183-194.
- Tamir S, Schwartz Y, Peleg U, Perez R, Sichel JY (2009) Acute mastoiditis in children: is computed tomography always necessary? Ann OtolRhinolLaryngol 118: 565-569.
- Hall P, Adami HO, Trichopoulos D, Pedersen NL, Lagiou P, et al. (2004) Effect of low doses of ionising radiation in infancy on cognitive function in adulthood: Swedish population based cohort study. BMJ 328: 19.
- Brenner DJ, Hall EJ (2007) Computed tomography-an increasing source of radiation exposure. N Engl J Med 357: 2277-2284.
- Bakhos D, Trijolet JP, Morinière S, Pondaven S, Al Zahrani M et al (2011) Conservative management of acute mastoiditis in children. Arch Otolaryngol Head Neck Surg 2011 137: 346-50.
- Gorphe P, de Barros A, Choussy O, Dehesdin D, Marie JP (2012) Acute mastoiditis in children: 10 year experience in a French tertiary university referral center. Eur Arch Otorhinolaryngol 269: 455-60.
- Mattos JL, Colman KL, Casselbrant ML, Chi DH (2014) Intratemporal and intracranial complications of acute otitis media in a pediatric population. Int J PediatrOtorhinolaryngol 78: 2161-4.
- Marom T, Roth Y, Boaz M, Shushan S, Oron Y et al (2016) Acute mastoiditis in children: Necessity and Timing of Imaging. Pediatr Infect Dis J 35: 30-4.
- Luntz M, Bartal K, Brodsky A, Shihada R (2012) Acute mastoiditis: the role of imaging for identifying intracranial complications.Laryngoscope 122: 2813-7.
- Minks DP, Porte M, Jenkins N (2013) Acute mastoiditis - the role of radiology. ClinRadiol 68: 397-405.
- Psarommatis I, Voudouris C, Douros K, Giannakopoulos P, Bairamis T, Carabinos C (2012) Algorithmic management of pediatric acute mastoiditis. Int J PediatrOtorhinolaryngol 76: 791-6.
- Psarommatis I, Giannakopoulos P, Theodorou E, Voudouris C, Carabinos C et al (2012) Mastoid subperiosteal abscess in children: drainage or mastoidectomy? J LaryngolOtol 126: 1204-1208.
- Enoksson F, Groth A, Hultcrantz M, Stalfors J, Stenfeldt K et al (2015) Subperiosteal abscesses in acute mastoiditis in 115 Swedish children. Int J PediatrOtorhinolaryngol 79: 1115-20.
- Chesney J, Black A, Choo D (2014) What is the best practice for acute mastoiditis in children? Laryngoscope 124: 1057-1058.
- Isaacson B, Mirabal C, Kutz JW Jr, Lee KH, Roland PS (2010) Pediatric otogenic intracranial abscesses. Otolaryngol Head Neck Surg 142: 434-437.
- Tov EE, Leiberman A, Shelef I, Kaplan DM (2008) Conservative nonsurgical treatment of a child with otogenic lateral sinus thrombosis. Am J Otolaryngol 29: 138-141.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences