Diagnosis of COVID-19 in a Child: A Challenge to Pediatricians
Sarah Assoni Bilibio*, Giovanna Belladona Ziani, Lucas Andreis, Lucas Bigarella Bracht and Daiane Vergani
Department of Medicine, University of Caxias do Sul, Caxias do Sul, Brazil
- *Corresponding Author:
- Sarah Assoni Bilibio
Department of Medicine,
University of Caxias do Sul, Caxias do Sul,
Brazil,
E-mail: sabilibio@ucs.br
Received date: December 30, 2022, Manuscript No. IPPIDO-23-15535; Editor assigned date: January 02, 2023, PreQC No. IPPIDO-23-15535 (PQ); Reviewed date: January 13, 2023, QC No IPPIDO-23-15535; Revised date: January 23, 2023, Manuscript No. IPPIDO-23-15535 (R); Published date: January 30, 2023, DOI: 10.36648/2471-9943.8.1.06
Citation: Bilibio SA, Ziani GB, Andreis L, Bracht LB, Vergani D (2023) Diagnosis of COVID-19 in a Child: A Challenge to Pediatricians. Pediatric Infect Dis Vol.8 No.1:06.
Abstract
Objective: Describing the Multisystem Inflammatory Syndrome (MIS-C) in children with COVID-19, in order to reinforce the importance of prevention.
Case description: Two cases were presented. The first one, the patient was referred for suspected appendicitis. An appendectomy was performed. Associated with the surgical complaint, the patient was isolated for suspected Coronavirus infection. During the hospitalization, he developed liver dysfunction; respiratory failure, requiring intubation; kidney failure; anasarca; electrolyte disturbances; severe respiratory acidosis and decreased pupillary reflexes. After performing the COVID-19 IgG/IgM rapid test, with reagent IgG, MIS-C was a suspected diagnosis. The patient developed multiple organ failure, dying from brain death. In the second case, the patient was referred to the service due to fever and red itchy patches on his body associated with an increase in cervical lymph nodes. The patient initially evolved with hemodynamic worsening, requiring intubation. After performing the positive COVID-19 IgG/IgM rapid test, the patient was diagnosed with MIS-C admitted to the pediatric ICU, he was medicated with human immunoglobulin. He was discharged in good general condition and good recovery.
Comments: According to the World Health Organization, MIS-C is characterized by a clinical condition compatible with the disease caused by the Coronavirus, with high markers of inflammation. The main clinical presentations reported in the pediatric population are fever and gastrointestinal symptoms. As in the reported cases, most cases of MIS-C end up evolving to mechanical ventilation for cardiovascular and respiratory stabilization due to the onset of sepsis. The prognosis of MIS-C is uncertain as it is a new clinical entity.
Keywords
Liver dysfunction; Respiratory failure; Requiring intubation; Kidney failure; Anasarca; Electrolyte disturbances
Introduction
Coronavirus disease is recognized as a public health problem. The virus that, at first, presented itself as a risk to the elderly, soon showed no distinction between age groups. In children, despite having a mild clinical manifestation with mild or asymptomatic cases, there are rare cases in which they can be severely affected.
It is known that SARS-CoV-2 is an enveloped β-Coronavirus that has an RNA genome and uses the Angiotensin-Converting Enzyme 2 (ACE2) as a receptor to invade cells. It is described that ACE2 is a membrane protein, expressed in many organs such as lungs, heart, kidneys and even in the digestive system. The infectivity of the new Coronavirus depends mainly on the affinity of its binding to the ACE2 receptor. In the pediatric population 57% demonstrate in addition to the classic symptoms linked to the respiratory system such as a cold, fever, runny nose, earache, sore throat and headache, children had gastrointestinal symptoms such as vomiting and diarrhea.
The period of active infection by COVID-19 is milder in children due to the high capacity for immune response. However, it was identified that the exacerbation of this response after infection triggers a severe systemic inflammatory response in the pediatric population Kawasaki Disease (KD), related to infection by COVID-19. One of the proofs of being a postinfectious syndrome is that it has often negative virological tests and only positive IgG antibodies. There are some similarities with KD and Staphylococcal Toxic Shock Syndrome (SCTE) such as fever, conjunctival blood vessel dilation, skin rash and oropharyngeal redness, but with differences in clinical, laboratory and epidemiological criteria of inflammatory syndrome secondary to COVID-19 infection MIS-C coursing with treatment in the ICU includes the use of immunoglobulin, glucocorticoids and prophylaxis for thromboembolism is suggested as treatment.
Case Description
Case 1
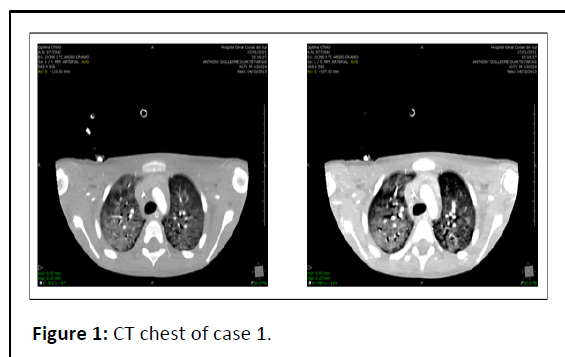
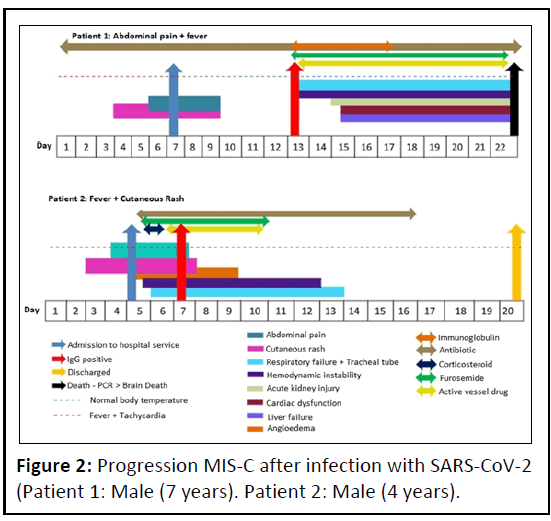
Patient referred from another hospital service for surgical evaluation due to suspicion of appendicitis. The patient had a distended abdomen, underwent analgesia and was referred to the operating room, where an appendectomy with mesenteric lymph node biopsy was performed. During the procedure, the appendix was identified with signs of inflammation, the presence of citrus-like free fluid and multiple enlarged mesenteric lymph nodes, which were referred for analysis. Associated with the complaint of appendicitis, the patient had a six-day history of fever, nausea, vomiting, loss of appetite, prostration, skin rash in the anterior cervical and face regionprobably associated with pharmacoderma and a drop in oxygen saturation (87%-90%). In addition, the patient was placed in isolation for suspected SARS-CoV-2 infection, since, in view of the surgical findings and clinical evolution of the patient, the family and personal clinical history was reviewed, which showed that the father of the child had a positive PCR for COVID-19 for one month. Laboratory tests indicated liver dysfunction, contributing to the suspicion of abdominal sepsis, starting antibiotic therapy with Linezolid and Meropenem. Chest X-ray showed the presence of diffuse and coarse bilateral infiltrate, but the patient initially did not present respiratory discomfort. The patient progresses with a significant worsening of the ventilatory pattern, and orotracheal intubation is performed. To relieve discomfort and agitation, sedation is performed with Midazolam, Phenobartital and Fentanyl. Patient is removed from isolation after a negative COVID-19 PCR result. A chest X-ray shows significant pleural effusion, and bilateral thoracentesis is performed and Furosemide is prescribed. The patient evolves with respiratory failure and worsening of renal function, with polyuria, even after volume restriction, with suspicion of Acute Renal Failure (ARF) in the polyuric phase. Due to persistent anemia, 1 CHAD transfusion is performed. Control chest X-ray persists with pleural effusion on the right, progressing to extensive consolidation in the right base, costophrenic sinus obliteration, and bilateral pleural effusion. Patient in septic shock, using vasoactive drugs due to hemodynamic instability, with persistence of liver alterations, electrolyte disturbances and severe respiratory acidosis. With the loss of pupillary reaction, suggesting neurological damage, a reduction in sedative doses is indicated. The patient evolves with a gradual decrease in diuresis, worsening of the Glomerular Filtration Rate (GFR) and multiple electrolyte disturbances. Due to the maintenance of hypercapnia, the patient needs an increase in ventilatory parameters. Due to a significant increase in blood glucose, 715 mg/dL, the application of regular insulin 0.1 UN/Kg/h is started. Once the diagnosis of ARF is confirmed, and with evolution to the oliguric phase, the Tenckoff catheter is placed in the lower right abdominal quadrant for peritoneal dialysis, since the replacement of Furosemide and Albumin did not have the expected response. The patient presents with anasarca and a large amount of purulent secretion in the upper airways. After performing a rapid IgG/IgM COVID-19 test, with reactive IgG, the patient is sent back for isolation. Suspecting pediatric multisystem inflammatory syndrome (P-SIM), the patient receives a dose of immunoglobulin. Dialysis is suspended, since there is no change in prognosis and clinical outcome. The patient remains with an absence of pupillary reflex, and continuous sedation is suspended. Patient evolves with Brain Death (BD) after performing the BD protocol as shown in Figure 1.
Case 2
Patient referred from another hospital service due to fever and itchy red spots on the body. Accompanied by her mother, this one reports the onset of fever four days ago- reaching a maximum temperature of 39°C and of the hyperemic and itchy spots for two days-which initially appeared in the groin region and subsequently reached the leg region, feet, hands and abdomen. Associated with these symptoms, he had enlarged cervical lymph nodes and no flu-like symptoms, vomiting, or diarrhea. At first, the patient presented tachypneic, febrile and severe angioedema. His exams showed the presence of anemia 8.3 g/dL hemoglobin-leukocytosis, 11,030 g/dL and thrombocytopenia 41,000 thousand/uL. Referred to the pediatric ICU, the patient received a pulse of Methylprednisolone, Oxacillin, Albumin and Furosemide, demonstrating a good response in reducing edema and increasing diuresis. After the first day of hospitalization, the patient evolved with hemodynamic worsening, requiring intubation; in addition, he had a significantly elevated CRP of 396.59. The use of Methylprednisolone was suspended, starting the use of Linezolid, Cefepime and epinephrine in low doses– requiring the association of noradrenaline in the following days, with a good response. The patient used mechanical ventilation for ten days due to the diagnosis of multisystem inflammatory syndrome, after confirmation of a positive IgG/IgM COVID-19 rapid test (IgG and IgM +), both for the child and for his mother. During the period of hospitalization in the ICU, it was decided to apply human immunoglobulin, even with the absence of evident signs of kawasaki-like on the cardiac ultrasound examination, following guidance from the epidemiological surveillance of the city. A post-extubation chest X-ray showed sub segmental atelectasis in the projection of the right middle lung field and thickening of the bronchial walls. After two weeks, the patient was discharged from the intensive care unit, remaining in the pediatric ward, in order to gradually withdraw from the sedative drugs in use, Clonidine, Lorazepam and Methadone, with good evolution, with only one isolated episode of fine tremors in the upper limbs. The patient evolved satisfactorily and was discharged from the hospital in good general condition, active and reactive, receiving an oral diet of solids and liquids without choking, with present bladder and intestinal eliminations and no abnormalities given by Figure 2.
Discussion
These case reports emphasize the embedded clinical course of two children admitted with recent SARS-CoV-2 infection and no comorbidities, presenting as hyperinflammatory syndrome and multiple organ dysfunction. According to the WHO, MIS-C is characterized by a clinical picture compatible with the disease caused by the Coronavirus, that is, high markers of inflammation, evidence of infection or contact with patients infected with COVID-19, presentation of a positive test for infection current or recent by SARS-CoV-2 or exposure to COVID-19 within 4 weeks before symptom onset and exclusion of other obvious microbial causes of inflammation [1-5]. In the cases described, it is possible to observe the follow-up to these recommendations, since they had reactive IgG on the 5th and 3rd day of hospitalization, respectively, and a history of contact with a recent PCR positive family member. However, preliminary data suggest that viral factors are less likely to explain why some children develop multisystem inflammation after SARS-CoV-2 infection, while others do not.
The main clinical presentations reported in the pediatric population are fever with an average duration of four to six days and gastrointestinal symptoms-abdominal pain, vomiting, and diarrhea-in almost 100% of the cases reported in the literature, which is compatible with the picture of both cases described. Less commonly, rash (45%-76%) is seen-present in both casesand conjunctivitis (30%-81%). Furthermore, 20%-55% of children had some involvement in the mucous membrane, neurocognitive symptoms, headache, lethargy, confusion-and respiratory symptoms [5-9].
Gastrointestinal symptoms are particularly common and prominent, presenting in some children similar to appendicitis. The first clinical case presented illustrates this entity: A condition that started with fever lasting an average of six days, associated with nausea and vomiting, on physical examination showed right lower abdominal pain and skin rash [2]. Appendicitis and a reactional pharmacoderma were suspected, however, the histopathological examination only showed a reactional follicular hyperplasia, which could be associated with an inflammatory reaction secondary to a viral infection [9].
As in the reported cases, most cases of MIS-C end up evolving to mechanical ventilation for cardiovascular and respiratory stabilization due to the onset of sepsis. Other notable features, in addition to persistent fever and exacerbated inflammatory activity, included the development of small pleural, pericardial and ascitic effusions, suggestive of a diffuse inflammatory process, as evidenced in the first report [6].
Laboratory findings are usually normal but may include leukopenia, lymphocytopenia, elevated procalcitonin, or elevated CRP. The first case reported presented laboratory tests consistent with an inflammatory process, highlighting the CRP values that reached 154 mg/dL and, in the second case, 396.59 mg/dL [4-6].
Imaging tests used for evaluation such as chest X-rays (X-ray) usually show pleural effusions, irregular consolidations, focal consolidation and atelectasis. Chest Computed Tomography (CT) shows findings similar to those of chest X-ray. Some patients, such as the one described in the first case, may present with nodular ground-glass pacification (Figure 1). On abdominal images, abdominal ultrasound or CT, the findings include free fluid, ascites and intestinal and mesenteric inflammation, including terminal ileitis, mesenteric adenopathy/adenitis and pericholecystic edema, findings that were also present in the examinations of the first patient [6-8].
In view of the evolution to hot vasoplegic shock, refractory to fluid resuscitation, norepinephrine and inotropic agents were needed, as well as immune modulation therapies and the use of high-dose corticosteroids, the treatment of choice used in both cases. The prognosis of MIS-C is uncertain as it is a new clinical entity, with long-term follow-up data still lacking. The overall mortality rate is approximately 1% to 2%, as was the outcome of the first patient reported, while the second presented an adequate response to the generalized inflammatory picture [9].
Conclusion
MIS-C is a diagnostic challenge, both because of its nonspecific clinical presentation and its ability to simulate other pathologies. As more is learned about it, it becomes evident that there is a spectrum of disease severity caused by the coronavirus, especially reactive to the post-infectious process, that is, pro-inflammatory that can lead to multiple organ failure and death from COVID-19, even after an active infectious process.
References
- Alfredo T, Cristina E, Santos M, Sanz-Samtaeugfemia FJ, Otheo E, et al. (2020) Screening and severity of Coronavirus disease 2019 (COVID-19) in children in Madrid, Spain. JAMA Pediatr 175: 316-317
- Xiaoxia L, Liqiong Z, Du H, Zhang J, Li YY, Qu J, et al. (2020) SARS-CoV-2 Infection in children. N Engl J Med 382: 1663-1665
- Liu W, Zhang Q, Chen J, xiang R, Song H, et al. (2020) Detection of COVID-19 in children in early January 2020 in Wuhan, China. N Engl J Med 382: 1370-1371
- Rowley AH (2020) Understanding SARS-CoV-2-related multisystem inflammatory syndrome in children. Nat Rev Immunol 20: 453-454.
- Feldstein LR, Rose EB, Horwitz SM, Collins JP, Newhams MM, et al. (2020) Multisystem inflammatory syndrome in U.S. children and Adolescents. N Engl J Med 383: 334-346
- Marcos APS, Cristina R (2020) Multisystem inflammatory syndrome in children and adolescents probably associated with COVID-19; an acute and potentially fatal presentation. Alert note from the Brazilian Society of Pediatrics.
- https://www.cdc.gov/mis/index.html
- Feldman SR, Freeman EE (2021) Clinical Manifestation of COVID-19 associated multisystem inflammatory syndrome in children and adolescentes, 2021–UpToDate.
- Feldman SR, Freeman EE (2021) Coronavirus disease 2019 (COVID-19): Cutaneous manifestation and issues related to dermatologic care. 2021–UpToDate.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences