Case Report of a V-P Shunt Dependent Child with Shunt Disconnection and Infection with Extended-Spectrum beta-Lactamase-Producing Klebsiella pneumoniae (ESBL-KP)
Rezina Hamid*and Sadeq Kawsar
DOI10.21767/2573-0282.100018
Rezina Hamid*and Sadeq Kawsar
Bangladesh Medical College Hospital, House 34/35, Road 14/A, Dhanmondi R/A, Dhaka-1209, Bangladesha
- *Corresponding Author:
- Rezina Hamid
Associate Professor of Neurosurgery
Bangladesh Medical College Hospital, House 34/35, Road 14/A, Dhanmondi R/A
Dhaka-1209, Bangladesh
E-mail: rezina.hamid@gmail.com
Received Date: March 25, 2016; Accepted Date: June 27, 2016; Published Date: June 30, 2016
Citation: Hamid R and Kawsar S (2016) Case Report of a V-P Shunt Dependent Child with Shunt Disconnection and Infection with Extended- Spectrum β-Lactamase-Producing Klebsiella pneumoniae (ESBL-KP). Pediatric Infect Dis 1:18. doi: 10.21767/2573-0282.100018
Abstract
Shunt malfunction superadded with infection in a shunt dependent child always lead to significant mortality and morbidity. Infections of central nervous system with Extended-Spectrum β-Lactamase-Producing Klebsiella pneumoniae (ESBL-KP) are very atypical, only occurs in immunosuppressive state and inappropriate treatment increases mortality and morbidity. Use of central catheter or ‘ommaya reservoir’ is a very good method of C.S.F drainage and intraventricular administration of some antibiotics. Here we report a shunt dependent baby of three and half years with history of recurrent respiratory tract infections, gastroenteritis and UTIs as she presented to us with shunt disconnection and simultaneous meningitis with Extended-Spectrum β-Lactamase- Producing Klebsiella pneumoniae (ESBL-KP). This patient was treated with removal of infected shunt, reservoir implantation, parenteral antibiotics and lastly reintroduction of V-P shunt with removal of ‘ommaya reservoir’.
Keywords
Ommaya reservoir; Intraventricular administration of antibiotic; Extended-Spectrum β-lactamaseproducing Klebsiella pneumonia; Shunt infection and disconnection
Abbreviations
ESBL-KP: Extended-Spectrum β-Lactamase-Producing Klebsiella pneumonia; CSF: Cerebrospinal Fluid; VPS: Ventriculo-Peritoneal Shunt, ETV: Endoscopic Third Ventriculostomy; ICP: Intracranial Pressure; CCS: Children Coma Scale; OFC: Occiputo-Frontal Circumference; ENT: Ear Nose Throat, UTIs: Urinary Tract Infections, CT: Computed Tomography, NPO: Nothing Per Oral, CNS: Central Nervous System, IVT: Intra Ventricular Therapy.
Introduction
Hydrocephalus occurs when there is excess production or most commonly due to decreased absorption of C.S.F. It may be consequence of aqueductal stenosis, meningitis, intracranial haemorrhage or brain tumour [1]. There are generally two approaches to treat hydrocephalus. The most common treatment is the placement of shunt in the form of ventriculoperitoneal, ventriculo-pleural or verticulo-atrial shunt [2]. The other procedure is Endoscopic Third Ventriculostomy (ETV), involves the surgical creation of an opening in the floor of the third ventricle to enable the passage of CSF into cistern [3,4]. Ventriculoperitoneal shunt is most commonly performed worldwide as a treatment of hydrocephalus [5]. Complications include shunt infection, shunt blockage or disconnection. Intra-abdominal complications include intestinal obstruction, gut perforation, pseudocyst formation [6-8]. Other complications reported in the literature include CSF ascites, inguinal hernia, and intestinal volvulus [9-11]. Infection remains a serious complication of shunt implantation, with a mortality rate ranging from 1.5–22% [12]. Those who survive are at risk intellectual, cognitive, and neurological deficits [13]. Infection has been reported to occur in 5–15% of shunt procedures [14-16]. However, some authors have described lower infection rates ranging from 0.3– 5% [17-21].
Many factors have been associated with shunt infection e.g. age of the patient, presence of infections. Most studies of the use of prophylactic antibiotic medications have given inconclusive results, and there has been no definite evidence that prophylactic antimicrobial medications reduce shunt infection rates. Other factors such as timing of the operation (elective/emergency), duration of surgery, number of operations/patient, number of people in the operation room, and length of time during which the shunt material is exposed to the atmosphere have been highlighted as contributing to shunt infection; these may all be included in specific “theatre discipline” [22]. Shunt mechanical complications may occur at any time from in the recovery room immediately after the shunt operation to years late [23]. The most common period for a shunt to fail is at the first 6 months after its insertion. Most common mechanical complication is the obstruction of CSF shunt flow and the accompanying rise in the cranial pressure. This rise leads most commonly to headache, nausea, vomiting and lethargy. Examination of the site of the shunt equipment implantation may provide confirmatory evidence of the shunt dysfunction [24]. Shunt infection remains as an important, distressing cause of shunt failure. Shunt removal with internal antibiotic treatment (usually with external ventricular drainage) carries the highest shunt infection cure rate and lowest mortality rate [25]. Developmental delay, poor cognitive function, visual and auditory defect may persist after treatment [26-29].
An Ommaya reservoir (Figure 1) is an intraventricular catheter system that can be used for the aspiration of cerebrospinal fluid or for the delivery of drugs (e.g. antibiotic, chemotherapy) into the ventricles. It consists of a catheter in one lateral ventricle attached to a reservoir implanted under the scalp [30-33].
Case Report
Baby “A”, a female child of three and half year was admitted to Bangladesh Medical College Hospital with fever, vomiting, irritability and deteriorating level of consciousness. On examination CCS level was 9 (E1 M5 V3), pupil small reacting, temperature 101oF and rigid neck. Abdomen was soft, nontender and shunt tube was felt disconnected at the occiput and there was fluid collection around the area of detachment.
She had a history of neonatal pyogenic meningitis (Flavobacterium, sensitive to ciprofloxacin) at the age of 45 days (OFC: 34 cm) and underwent VP shunt surgery due to post meningitic hydrocephalus (OFC: 43 cm). Within 2 month of operation shunt became disconnected and a revision surgery was done. During the growing period parents noticed that the baby unresponsive to sound and was taken to ENT hospital, diagnosed as a case of sensory neural deafness. Another episode of shunt revision for migration of peritoneal end of catheter into the peritoneal cavity was done after ten months of first revision. Since these, she has been receiving treatment several times as case for impetigo, tonsillitis, recurrent pneumonia and UTIs by the pediatricians.
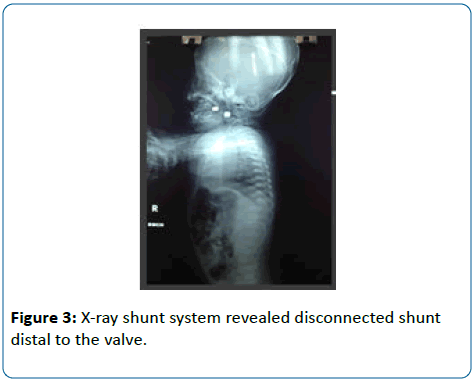
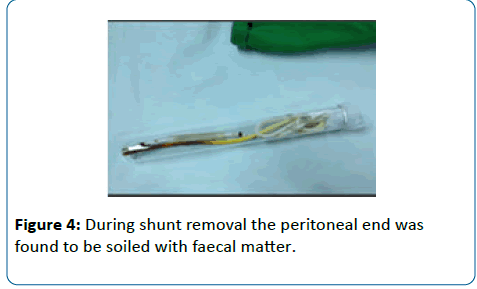
Now this time, investigation showed neutrophilic leukocytosis. CT scan of brain revealed cranial end of shunt tube placed in situ with dilated ventricles and compressed brain matter (Figure 2). X-ray shunt system revealed disconnected shunt distal to the valve (Figure 3). We diagnosed her as a case of “shunt failure”. The baby underwent shunt removal, attempted ETV with Ommaya reservoir placement. During shunt removal the peritoneal end was found to be soiled with faecal matter (Figure 4) and cranial end was stubbornly attached with (?) Choroid Plexus which was dislodged with the help of monopolar cauterization. We tried ETV in this session but third ventricular floor was opaque and thickened with hazy CSF and scarred Choroid plexus and aqueduct was stenosed. It was impossible to form a stoma for minimizing intra cranial pressure. We put an Ommaya reservoir through the right frontal burr hole and shunt tube was sent for culture and sensitivity. Post operatively we kept the patient NPO for high suspicion of intestinal perforation. Plain X-ray abdomen erect posture revealed nothing significant throughout the period. Abdomen was soft and non-tender. In the meantime baby was treated with regular 20-30 cc CSF aspiration and 1 mg gentamicin and 5 mg vancomycin in intraventricular route and metronidazole 7.5 mg/kg, 8 hourly in intravenous route. After culture and sensitivity test we stopped all of previous antibiotic and switched to meropenem. As culture of shunt tube was found to be growth of profuse Klebsiella pneumoniae which was which was found sensitive to meropenem, imipenem, amikacin, piperacillin-tazobactam. Baby became apyrexic and neck rigidity resolved soon. After 14 days CSF became clear, it was culture negative and complete blood count became normal baby was stable.
Then we did left side VP shunt (opposite side of previous burr hole) with removal of ommaya reservoir. Post-operative period was uneventful and the baby was discharged after 10 days. After 6 months of surgery baby was doing fine.
Discussion
Ventriculoperitoneal shunt associated CNS infection may be caused by overlying skin breakdown, bacteremia due to some systemic disease, colonization of shunt tube during surgery or retrograde infection from distal end of shunt. Patient may present with fever, depressed consciousness, redness over the shunt line, sign of peritonitis [34-36]. In this case, the patient had ESBL-KP shunt infection and retrograde ventriculitis. Infection with ESBL producing organisms needs state of immunosuppression. It may be aggravated by repeated respiratory/urinary tract infections, malignancies, prolonged hospital stay and use of broad spectrum antibiotics [37]. Removal of infected hardware along with antibiotic treatment showed the best result. On the basis of these findings, the authors concluded that the treatment combination of shunt removal, 20 mg/d of intraventricular vancomycin, and systemic antibiotics was both safe and effective for CSF shunt infections [38].
Endoscopic third ventriculostomy (ETV) is currently considered as the best treatment for obstructive hydrocephalus. Obstruction is most frequently at the level of aqueduct. It may result from congenital blockage, post meningitic state intraventricular hemorrhage or posterior fossa space occupying lesion [39]. We tried endoscopic procedure but circumstances were not favorable.
Extended-spectrum beta-lactamases (ESBLs) producing organisms are capable of hydrolyzing beta lactum antibiotics like ceftriaxone, ceftazidime. They are most commonly found in Klebsiella pneumoniae [40]. Carbapenems (imipenem or meropenem) should be the drug of choice, other beta lactam antibiotics (cefepime) are not suitable as first line antibiotics [41,42].
Conclusions
Repeated respiratory tract infection and other systemic infections in a shunt dependent patient may results shunt infection with rare pathogens. Removal of infected hardware, creating an alternate pathway for CSF drainage and administration of meropenem and intraventricular gentamicin delivered good result. Placement of Ommaya reservoir was very useful for removal of cerebrospinal fluid and introducing intraventricular antibiotics. Finally, shunt surgery should be done by expert hand and unnecessary cutting and reconnecting of shunt tube should be avoided.
References
- Benjamin CW, Lynda MacGowen RN Post infectious hydrocephalus: The Most Common Cause of Hydrocephalus; if HSB; International federation for hydrocephalus and spina bifida, Consultative status special category with Economic and Social Council of the United Nations Consultative status, Council of Europe .
- Kandasamy J, Jenkinson MD, Mallucci CL (2011) Contemporary management and recent advances in paediatric hydrocephalus. BMJ 343: 146-151.
- Yadav YR, Parihar V, Pande S, Namdev H, Agarwal M (2012) Endoscopic third ventriculostomy. J Neurosci Rural Pract 3: 163-173.
- Moorthy RK, Rajshekhar V (2011) Endoscopic third ventriculostomy for hydrocephalus: a review of indications, outcomes, and complications. Neurol India 59: 848-854.
- Borgbjerg BM, Gjerris F, Albeck MJ, Hauerberg J, Børgesen SE (1995) Frequency and causes of shunt revisions in different cerebrospinal fluid shunt types. ActaNeurochir (Wien) 136: 189-194.
- Sells CJ, Shurtleff DB, Loeser JD (1977) Gram-negative CSF shunt associated infections. Pediatrics 59: 614: 618.
- Acharya R, Ramachandran CS, Singh S (2001) Laparoscopic management of abdominal complications in ventriculoperitoneal shunt surgery. J LaparoendoscAdvSurg Tech 11: 167-170.
- Wani AA, Ramzan A, Wani MA (2002) Protrusion of a peritoneal catheter through the umbilicus: an unusual complication of a ventriculoperitoneal shunt. PediatrSurgInt 18: 171-172.
- Nfonsam V, Chand B, Rosenblatt S, Turner R, Luciano M (2008) Laparoscopic management of distal ventriculoperitoneal shunt complications. SurgEndosc 22: 1866-1870.
- Bal RK, Singh P, Harjai MM (1999) Intestinal volvulus: a rare complication of ventriculoperitoneal shunt. PediatrSurgInt 15: 577-578.
- Sathyanarayana S, Wylen EL, Baskaya MK, Nanda A (2000) Spontaneous bowel perforation after ventriculoperitoneal shunt surgery: case report and a review of 45 cases. SurgNeurol 54: 388-396.
- Welch K (1979) Residual shunt infection in a program aimed at its prevention. Z KinderchirGrenzgeb 28: 374-377.
- Shurtleff DB, Foltz EL, Loeser JD (1973) Hydrocephalus. A definition of its progression and relationship to intellectual function, diagnosis, and complications. Am J Dis Child 125: 688-693.
- Gardner P, Leipzig T, Phillips P (1985) Infections of central nervous system shunts. Med Clin North Am 69: 297-314.
- Schoenbaum SC, Gardner P, Shillito J (1975) Infections of cerebrospinal fluid shunts: epidemiology, clinical manifestations, and therapy. J Infect Dis 131: 543-552.
- Shurtleff DB, Stuntz JT, Hayden PW (1985) Experience with 1201 cerebrospinal fluid shunt procedures. PediatrNeurosci 12: 49-57.
- Ajir F, Levin AB, Duff TA (1981) Effect of prophylactic methicillin on cerebrospinal fluid infections in children. Neurosurgery 9: 6-8.
- Duret N, Derex MC, Chacornac R (1983) Essai de prevention des risquesinfectieux au cours des traitements de l’ hyalo-rachidien. Agressologie 24: 239-242.
- Fitzgerald R, Connolly B (1984) An operative technique to reduce valve colonization. Z Kinderchir 39: 107-108.
- Haines SJ, Taylor F (1982) Prophylactic methicillin for shunt operations: effects on incidence of shunt malfunction and infection. Childs Brain 9: 10-12.
- Walters BC, Hoffman HJ, Hendrick EB (1984) Cerebrospinal fluid shunt infection. J Neurosurg 60: 1014-1021.
- Welch K (1979) Residual shunt infection in a program aimed at its prevention. Z Kinderchir 28: 374-377.
- Choksey MS, Malik IA (2004) Zero tolerance to shunt infections: can it be achieved? J NeurolNeurosurg Psychiatry 75: 87-91.
- Drake JM, Kestle J (1996) Determining the best cerebrospinal fluid shunt valve design: the pediatric valve design trial. Neurosurgery 38: 604-607.
- James M, Drake, Iantosca R (2002) Current systems for cerebrospinal fluid shunting and management of pediatrichudrocephalus:endoscopic and image guide surgery in hydrocephalus. Operative neurosurgical techniques of Schmidek and Sweet. 4th edn., pp 573-594.
- James HE, Walsh JW, Wilson HD, Connor JD, Bean JR, et al. (1980) Prospective randomized study of therapy in cerebrospinal fluid shunt infection. Neurosurgery 7: 459-463.
- Hattingen E, Jurcoane A, Melber J, Blasel S, Zanella FE, et al. (2010) Diffusion tensor imaging in patients with adult chronic idiopathic hydrocephalus. Neurosurgery. 66: 917-924.
- Hamilton MG (2009) Treatment of hydrocephalus in adults. SeminPediatr Neurol. 16: 34-40.
- Woodworth GF, McGirt MJ, Williams MA, Rigamonti D (2009) Cerebrospinal fluid drainage and dynamics in the diagnosis of normal pressure hydrocephalus. Neurosurgery 64: 919-925.
- Lacy M, Oliveira M, Austria E, Frim MD (2009) Neurocognitive outcome after endoscopic third ventriculocisterostomy in patients with obstructive hydrocephalus. J IntNeuropsycholSoc 15: 394-398.
- Partington MD (2001) congenital hydrocephalus. NeurosurgClin N Am 12: 737-742.
- Vinchon M, Rekate HL, Kulkarni AV (2012) Pediatric hydrocephalus outcomes: a review. Fluids Barriers CNS 9: 18.
- DeBenedictis CN, Rubin SE, Kodsi SR (2015) Esotropia in Children with Ventricular-Peritoneal Shunts. Strabismus 23: 117-120.
- Oertel JM, Mondorf Y, Baldauf J, Schroeder HW, Gaab MR (2009) Endoscopic third ventriculostomy for obstructive hydrocephalus due to intracranial hemorrhage with intraventricular extension. J Neurosurgpp 8.
- Espay AJ, Narayan RK, Duker AP, Barrett ET Jr, de Courten-Myers G (2008) Lower-body parkinsonism: reconsidering the threshold for external lumbar drainage. Nat ClinPractNeurol 4: 50-55.
- Larsson A, Moonen M, Bergh AC, Lindberg S, Wikkelso C (1990) Predictive value of quantitative cisternography in normal pressure hydrocephalus. ActaNeurolScand 81: 327-332.
- Walchenbach R, Geiger E, Thomeer RT, Vanneste JA (2002) The value of temporary external lumbar CSF drainage in predicting the outcome of shunting on normal pressure hydrocephalus. J NeurolNeurosurg Psychiatry 72: 503-506.
- Leonidas C. Goudas et al (1999) Acute Decreases in Cerebrospinal Fluid Glutathione Levels after Intracerebroventricular Morphine for Cancer Pain, International Anesthesia Research Society 1999. Anesthesia & Analgesia 89: 1209-1215.
- Van de Beek D, Drake JM, Tunkel AR (2010) Nosocomial bacterial meningitis. N Engl J Med 362: 146-154.
- Yaita K, Komatsu M, Oshiro Y, Yamaguchi Y (2012) Post-operative meningitis and epidural abscess due to extended-spectrum beta-lactamase-producing Klebsiellapneumoniae: a case report and a review of the literature. Intern. Med 51: 2645-2648.
- Davis SE, Levy ML, McComb JG, Masri-Lavine L (1999) Does age or other factors influence the incidence of ventriculoperitoneal shunt infections? PediatrNeurosurg 30: 253-257.
- Yadav YR, Parihar V, Pande S, Namdev H, Agarwal M (2012) Endoscopic third ventriculostomy. J Neurosci Rural Pract 3: 163-173.
- Paterson DL (2000) Infectious Disease Section, Instituto per I TrapiantiTerapie as Alta Specializzazione, Palermo, Italy and Infectious Disease Division, University of Pittsburgh Medical Center, Pittsburgh, USA. ClinMicrobiol Infect 6: 460-463.
- Paterson DL (2000) Recommendation for treatment of severe infections caused by Enterobacteriaceae producing extended-spectrum beta-lactamases (ESBLs). ClinMicrobiol Infect 6: 460-463.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences