An Extended Snapshot of STI Screening at Royal Darwin Hospital of Paediatric Patients Aged 12-16: A Five-Year Retrospective Study from 2015-2020
Tayler Cosentino* and Peter Wallis
Published Date: 2024-01-03Tayler Cosentino* and Peter Wallis
Department of Pediatric, Royal Darwin Hospital, Rocklands, Australia
- *Corresponding Author:
- Tayler Cosentino
Department of Pediatric,
Royal Darwin Hospital,
Rocklands,
Australia,
Tel: 0401164445;
E-mail: taylersian@gmail.com
Received date: June 06, 2023, Manuscript No. IPPIDO-23-16941; Editor assigned date: June 09, 2023, PreQC No. IPPIDO-23-16941 (PQ); Reviewed date: June 26, 2023, QC No. IPPIDO-23-16941; Revised date: December 27, 2023, Manuscript No. IPPIDO-23-16941 (R); Published date: January 03, 2024, DOI: 10.36648/2573-0282.9.1.001
Citation: Cosentino T, Wallis P (2024) An Extended Snapshot of STI Screening at Royal Darwin Hospital of Paediatric Patients Aged 12–16: A Five- Year Retrospective Study from 2015-2020. Pediatric infect Dis Vol:9 No:1
Abstract
Aim: To determine the rate at which adolescent patients presenting to Royal Darwin Hospital (RDH) are screened for sexually transmitted infections and describe the results of those screened.
Methods: A retrospective five year audit of STI testing in children aged 12-16 years old; who presented to RDH between 2015 and 2020 was conducted. Laboratory data was obtained for STI tests ordered for children within the age range during the study period and compared with patient separation data to ascertain: The proportion of children who were screened for an STI, the proportion of those who were screened that tested positive for an STI and what STIs were detected.
Results: In total 11,145 children between the ages of 12 and 16 presented to RDH over the five years and 542 (5%) adolescents were tested for STIs. Of this population, 84 adolescents (15%) tested positive for an STI. 32% of patients with an STI detected tested positive for more than one STI. Patients who were fifteen years old tested positive most frequently regarding absolute numbers as well as proportion. Almost 75% of the patients tested and 94% of the patients with a positive result were female.
Discussion: There is a high prevalence of STIs in pediatric patients tested at Royal Darwin Hospital with high co infection rates. Hospital admission may represent an opportunity for screening adolescents for STIs, and further consideration should be given to groups who may be screened.
Keywords
STI; Paediatric; Adolescent; Sexual health; Children
Introduction
STIs are a significant source of female reproductive morbidity, with infections being associated with Pelvic Inflammatory Disease (PID), tubal factor infertility and chronic pelvic pain [1]. These infections are becoming increasingly common in the adolescent population. The longitudinal study of Australian children ‘growing up in Australia’ which follows 10,000 young people and their families for nearly 20 years suggests one third of Australian youth aged 16-17 years old are sexually active [2]. The same research suggests one fifth of sexually active adolescents are not actively trying to prevent STIs through preventative strategies like condom use. National guidelines recommend twice annual STI testing in sexually active young people with special emphasis on high risk groups including Aboriginal youth [3].
The Northern territory is a hyper endemic region for STIs. And this issue disproportionately affects young aboriginal and Torres Strait islander (Aboriginal from here onwards) people [4]. With notification rates for chlamydia, gonorrhea and syphilis up to 50 times higher for aboriginal youth living in remote and very remote areas compared to their non-Aboriginal urban dwelling peers [4]. The Royal Darwin Hospital (RDH) acts as the principal tertiary hospital of the top end and services a population of 140, 000 people 50% of whom live in remote and very remote areas [5]. When considering the unique healthcare landscape of the NT and adolescents being groups that often fail to regularly access primary health care the RDH acts as a possible catchment service for sexually active paediatric patients who would otherwise not be screened for STIs [6].
This paper aims to provide a snapshot of clinical practice regarding STI testing at the RDH for paediatric patients aged 12-16.
Brief points
STIs represent a noteworthy source of reversible morbidity in young people with serious complications like PID and infertility.
Young people may struggle to access sexual health services due to barriers like access and fears over confidentiality. There may also be a general lack of education surrounding safe sexual practices and the necessity of regular STI testing in younger patients. These barriers are especially obvious when considering the remote health landscape of the NT where there are limited primary health services.
Youth in the northern territory, particularly aboriginal and Torres Strait islander youth are at an increased risk of testing positive for STIs. With notification rates for gonorrhea, chlamydia and syphilis up to 50% higher for Aboriginal youth living in remote and very remote areas compared to urban nonaboriginal peers.
By following pediatric presentations over five years, this paper contributes an extended snapshot of the sexual health of young people in the NT. In addition to the increased context of the wider community, this clinical audit adds information regarding rates of STI testing by RDH laboratory and the positive predictive value of such testing by highlighting patients most at risk (i.e. female patients aged 15).
Materials and Methods
Ethics approval was granted by the human research ethics committee of the Northern Territory department of health before the study commencement.
This clinical audit was conducted on STI testing in adolescents aged 12–16 years in all wards at RDH and the Emergency Department (ED) from 1st January 2015 to 31st December 2019. Demographics included were limited to age and gender. The STIs investigated in this audit were chlamydia, gonorrhoea, trichomonas, syphilis and HIV; these infections were selected due to their prevalence in the top end in accordance with the ‘NT management guidelines for STIs in the primary health care setting’ [6]. The primary outcome of interest was the proportion of patients who presented to RDH who were tested and the proportion of positive results from STI investigations; secondary outcomes included co infection rates or re infection within the same individual.
A list of all samples tested for chlamydia, trichomonas, syphilis and HIV for any patient aged between 12 and 16 years old from any location within RDH (excluding outpatients) inside the dates of 1st January 2015 to 31st December 2019 were obtained from the RDH laboratory register. Of note, patients who provided samples in ED and were discharged directly from the department without inpatient admission were still included in the study. Patients who did not fit these criteria were excluded from the study. The number of hospital separations for children between the ages of 11 and 16 years in the same period was obtained from patient records.
Results for chlamydia, trichomonas and gonorrhoea were based on PCR testing and divided by positive results (results were an STI was detected), negative results (an STI was not detected), samples which were not tested (due to inadequate collection or other reasons) and in determinant results (STI status could not be excluded or included based on a sample provided). Testing for HIV and syphilis was based on titres. The data was then analysed using simple descriptive statistics.
Results
In total, of the 11,145 patients aged 12–16 who presented to RDH over the five years, 5% (542 patients) were tested for an STI with 15% of this tested population testing positive. Almost three quarters of patients tested were female (74%) and this was represented in positive results with 95% of patients who tested positive being female.
Gonorrhoea was most frequently requested with an average of 123 tests per year (616 tests ordered in total) and 63 total positive results. Testing for trichomonas also found 63 positive results over the five years with consistent rates of testing (597 tests in total). Syphilis testing rates increased with a total of 247 tests ordered and positive test results for 15 patients. Data for chlamydia testing in 2015 was unavailable due to a system change over at the time and the low rates of testing in 2016 (12 tests) likely indicate ongoing data loss rather than low testing rates. However, over four years, a total of 391 tests were ordered, positive results were returned on 35 patients. No HIV was detected in adolescent patients during this time with a total of 73 tests.
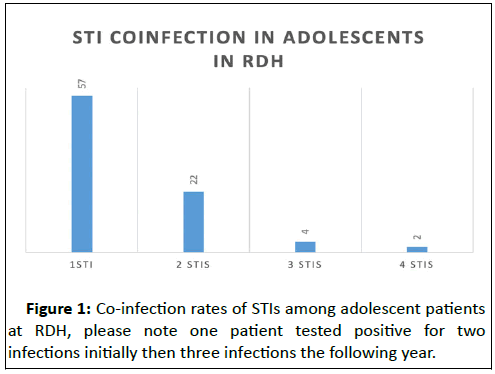
Over five years, RDH detected 84 positive patients with 32% of infected individuals testing positive for multiple STIs simultaneously. Whilst the large majority of co infection was limited to two STIs, 22% of patients had three or more infections with two female patients (aged 14 and 15) testing positive for four infections simultaneously (Figure 1). Overall, 27 patients accounted for 40% of the total disease burden detected.
From the data, it is evident 15-year-old female patients tested positive for all STIs most frequently, regarding both absolute numbers (65 STIs detected) as well as by population proportion testing positive (12.7%). Patients who were 14 and 12 were second most likely to test positive regarding positive proportions with 9.8% of patients testing positive but 16 year old individuals had greater numbers of STIs detected (Table 1).
| Age tested | Total tests ordered | Total tests positive | % positive testing |
|---|---|---|---|
| 12 years old | 132 | 13 | 9.8 |
| 13 years old | 184 | 13 | 7.1 |
| 14 years old | 417 | 41 | 9.8 |
| 15 years old | 513 | 65 | 12.7 |
| 16 years old | 667 | 44 | 6.6 |
Table 1: STI testing detection rates by age of the patient.
However, of the 176 total STIs which were detected by RDH, only four patients tested positive for re-infection with the same STI at a later date. Two patients tested positive for re-infection with trichomonas and two patients had positive results for syphilis.
Discussion
This clinical audit found over five years only 5% of pediatric patients who presented to the hospital for healthcare were tested for STIs. This low percentage of testing likely represents investigative settings with high clinical suspicion rather than opportunistic screening. This proportion of testing is somewhat reasonable considering the hospital setting and STI diagnosis being lent more to a primary health care setting. However, as previously discussed the unique healthcare landscape of the NT combined with an adolescent aversion to regular GP contact raises the question of whether RDH can operate as a possible catchment for some of these patients. Additionally, as previous research suggests one third of adolescents are sexually active inpatient admission could represent a possible intervention moment with increased rates of testing and education.
Considering the proportion of patients who tested positive was 15% and a large group were positive for multiple STIs, rates of detection for STIs at RDH were high. As previously speculated, this is likely due to patient presentation directed investigations e.g. abdominal pain in a 15 years old female. The bias in this population is further obvious considering nearly three quarters of the sample were female. The significant discrepancy between male and female testing may be explained by broader clinical indication and other factors such as routine testing on the obstetric ward and greater motivation to discuss sexual health considering pregnancy risk. It is apparent that older pediatric patients, aged 15-16, are most at risk of testing positive for STIs and having multiple infections simultaneously. However, evidence from the data is some adolescents are becoming sexually active very early and this should be considered when treating pediatric patients.
These findings can be compared with existing literature on the topic, compared to the ACCESS study performed by the Kirby Institute on STI rates diagnosed in community clinics in the NT7. While similar positive rates of chlamydia were detected, our clinical audit had higher rates of gonorrhea, trichomonas, and syphilis diagnosed [7]. This may perhaps be due to testing in the hospital being more investigative and diagnostic than the opportunistic screening of high risk patients.
Clinically, these findings demonstrate that pediatric patients may be sexually active, and clinicians should be encouraged to take sexual histories and perform appropriate opportunistic or investigative screening of these patients. The sexually active adolescent raises concerns for sexual abuse and coercion, early sexual debut and the risk of unplanned pregnancy in a pediatric patient. The morbidity associated with STIs can be severe with complications like PID and tubal factor infertility hence this data is alarming when considering the young age of these patients and the compounding risk of re infection in the coming decades. The alarming rates of co-infection represent a heavy disease burden for a small population of patients, which has significant potential short and long term morbidity. While primarily considered a community intervention, the importance of testing for STIs in a hospital setting should not be understated, especially in a hospital that services such a remote population.
This audit had noteworthy limitations impacting the interpretation of the data. By only focusing on hospital admissions and ED presentations, a significant proportion of patients were likely tested in outpatient clinics and communitybased health settings. For example, while this audit demonstrated only 2 adolescents became re-infected with the same STI, patients may have been become re infected and been investigated and treated in the outpatient setting. This is likely considering the focus on STI intervention in the community setting rather than a hospital focus [8,9]. Another limitation was the lack of indication for STI testing; it is unclear if patients were tested for investigatory reasons due to symptoms and clinical suspicion or opportunistic holistic health care. Finally, it would be interesting to expand the data to include more demographics for these patients, for example, Aboriginal or Torres Strait Islander identity [10].
Conclusion
This retrospective clinical audit focused on STI testing in the adolescent population at RDH over five years. In total, 11,145 patients aged 12–16 years old presented to RDH, of this population 5% (542 patients) were tested for an STI. Positive test results were returned for 84 patients with patients most at risk being 15–16 years old females. This audit found significant rates of co infection among the pediatric population, with 27 individuals being responsible for 40% of the total STIs burden.
Whilst co infection was largely limited to two STIs some individuals had three or four STI's simultaneously. This represents significant morbidity in the pediatric population. Testing for STIs is an essential aspect of sexual health in adolescents, but reliable, long lasting contraception and education surrounding safe sexual practices and consent should also be discussed and encouraged. This clinical audit is acting as a pilot study for which further research may be based.
Recommendations
Recommendations stemming from this audit's outcome are limited to the primary objective; screening and investigating adolescents for STI who present or are admitted to the hospital. Young as twelve years old are sexually active and are, therefore, at risk for acquiring STIs.
• Adolescents who present to the hospital for healthcare should
be asked about their sexual history and, if sexually active,
should be considered for STI testing. A sexual history with
consideration of opportunistic STI screening is especially
relevant for patients who are from remote communities where
the prevalence of STIs is much greater.
• When testing for one STI, consider testing for a panel of
common STI's including chlamydia, gonorrhoea, trichomonas,
syphilis and HIV.
• Given the high incidence of STIs noted consideration should be
given for routine testing for STIs in children in high-risk groups
on admission to the hospital.
Ethics Approval
Menzies institute HREC 2020-3682.
References
- Warren D, Swami N (2018) Teenagers and sex. LSAC annual statistical report 2018. 47-56
- Bell S, Aggleton P, Ward J, Murray W, Silver B, et al. (2020) Young Aboriginal people’s engagement with STI testing in the Northern Territory, Australia. BMC Pub Health 20:1-9
- Kang M, Robards F, Luscombe G, Sanci L, Usherwood T (2020) The relationship between having a regular general practitioner (GP) and the experience of healthcare barriers: A cross-sectional study among young people in NSW, Australia, with oversampling from marginalised groups. BMC Fam Pract 21:1-9
[Crossref] [Google Scholar] [PubMed]
- Challander D, Donovan B, Guy R (2015) The Australian collaboration for coordinated enhanced sentinel surveillance of sexually transmissible infections and blood borne viruses: NSW STI Report 2007-2014. Sydney, Australia: University of New South Wales, Australia.
- Burke E, Gold J, Razafinirinasoa L, Mackay A. Youth voucher program in Madagascar increases access to voluntary family planning and STI services for young people. Glob Health Sci Pract 5:33-43
[Crossref] [Google Scholar] [PubMed]
- Zheng W, Anderson SF, Kriss GA, Chiu K, Haggard D, et al. (2005) Progress in studies of intergalactic He II absorption. Proceedings of the International Astronomical Union 1:484-486
- Ogunbodede OT, Zablotska-Manos I, Lewis DA (2021) Potential and demonstrated impacts of the COVID-19 pandemic on sexually transmissible infections: Republication. Curr Opin HIV AIDS 16:115-120
[Crossref] [Google Scholar] [PubMed]
- Deans AK, Boerma CJ, Fordyce J, de Souza M, Palmer DJ, et al. (2013) Use of Royal Darwin Hospital emergency department by immigration detainees in 2011. Med J Aust 199:776-778
[Crossref] [Google Scholar] [PubMed]
- Parameswaran U, Baird RW, Ward LM, Currie BJ (2012) Melioidosis at Royal Darwin Hospital in the big 2009–2010 wet season: Comparison with the preceding 20 years. Med J Aust 196:345-348
[Crossref] [Google Scholar] [PubMed]
- Stephens DP, Thomas JH, Ward LM, Currie BJ (2016) Melioidosis causing critical illness: A review of 24 years of experience from the Royal Darwin Hospital ICU. Crit Care Med 44:1500-1505
[Crossref] [Google Scholar] [PubMed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences